Less is more: lung-sparing direct repair of a traumatic rupture of the bronchus intermedius
Introduction
Nowadays, thoracic trauma accounts for about 25% of traumatic deaths, and it is a contributory factor in a further 50%, usually because of hypoxia and/or hypovolemia (1). Blunt chest trauma is by far more devastating and fatal than penetrating chest trauma since it is typically more extensive and it is frequently associated with major injuries to vital organs outside the thorax (2,3). Tracheobronchial injuries are often related to penetrating trauma. On the contrary, they are rarely associated with blunt chest trauma due to high-energy impacts (such as in high-speed traffic crashes) (4). Most patients die on the scene of the accident. Leading causes of death are ineffective airway management, tension hemopneumothorax, air embolism and major cardiac or vascular lacerations. Since hypoxemia represents the major consequence of thoracic trauma, early intervention and advanced management of airway are the keys to survival. Once in the hospital, if the patient is hemodynamically stable, conservative and lung-sparing techniques should be treatments of choice (5), but major pulmonary resections, pneumorraphy, lung packing, an emergency thoracotomy can be necessary in the case of extensive injuries with deep lacerations or involvement of bronchi and vessels (6). The typical clinical features include dyspnoea and hemopneumothorax with continuous air leak that is refractory to the placement of chest drainage (7). In very few cases, treatment of shock and hypoxemia may even require a resuscitative thoracotomy [usually performed inside the emergency room (ER)], but survival rate after blunt trauma is less than 1%.
Case presentation
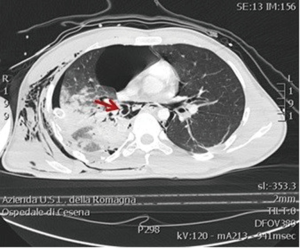
Here we report the case of a 25-year-old man who suffered the injury of the right middle bronchus. In September 2016, he was admitted to our Trauma Center—Level I after a severe motorcycle crash in which he was thrown about 10 meters away after the hit of a car. The injury severity score (ISS) was 35 at the admission. On the accident scene, the patient was conscious with a Glasgow Coma Scale (GCS) of 13 but dyspnoeic with chest pain and shortness of breath. He was hypotensive (blood pressure =95/45 mmHg) and tachycardic (heart rate =125 bpm). At the primary survey, a right flail chest with pneumothorax was shown therefore he was immediately intubated. A needle decompression of the pleural cavity was performed without clinical improvements. The Emergency Blood Transfusion Protocol (immediate availability of 4 red blood cells units in ER shock room) was activated on scene by the emergency physician. The patient was referred to our hospital by helicopter in about 30 min after the accident. In our ER shock room, he arrived hypoxemic with an oxygenation ratio (PaO2/FiO2) =130 and still hypotensive, and first blood gas analysis yielded pH =7.32, PaCO2 =42, arterial lactate =1.4, BE =−5.2, Hb =14.2. To prevent trauma-related coagulopathy, 2 g of fibrinogen and tranexamic acid were administrated. Chest examination showed not audible right breath sounds and palpable extensive subcutaneous crepitus. Initial plain chest roentgenogram revealed multiple rib fractures and a collapsed right lung. The surgeon immediately inserted a large bore chest drainage with heavy air and blood output (about 700 mL). The urgent whole body computed tomography (CT) scan demonstrated a right hemopneumothorax with pneumomediastinum (Figure 1). Subcutaneous emphysema and massive air leakage continued, and an additional large bore chest drainage was positioned. An unstable and floating right shoulder (both scapula and clavicle fractures) was also associated without involving subclavian vessels. Also, the patient had facial trauma, right costal fractures, deep, extensive pulmonary lacerations and six uncomplicated thoracic vertebral transverse process fractures.
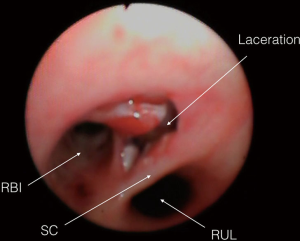
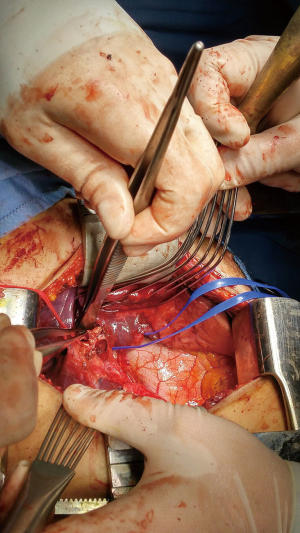
The high-energy nature of the crash, the continuous severe air leak and the failure of lung expansion despite the double chest drainage insertion, suggest a tracheobronchial injury (8) and bronchoscopy is the most effective method to diagnose (2,9). A bedside emergent bronchoscopy was performed, and the right middle bronchus laceration was identified, less than 2 cm involving the whole thickness of the wall (Figure 2). As a first procedure, a bronchial blocker was positioned in the right main bronchus to achieve one lung ventilation. An extensive lung damage with urgent lobar or pulmonary resection increases the mortality rate to 43% (9). Since the patient was hemodynamically stable, it was decided a parenchyma-sparing operation. Both the endotracheal tube and the bronchial blocker were removed and left sided 39 Fr double lumen tube (RobertShaw endobronchial tube, Rusch, NY, USA) was inserted under bronchoscope vision; a thoracic epidural catheter for postoperative pain management was positioned. The patient underwent an urgent right posterolateral thoracotomy about 6 h after arrival. Thoracic surgeon realised a challenging conservative intervention with a bronchoplastic procedure. The bronchial stump was repaired with a continuous running 4-0 Prolene (Ethicon, Somerville, NJ, USA) suture (Figure 3). A pericardial fat flap was buttressed over the bronchus to protect the stitching, and the two-lung ventilation was successfully resumed. There was no direct air leakage through the anastomosis site after recruitment manoeuvres at a positive pressure of 40 cm H2O. Therefore, the double lumen tube was immediately removed, and an endotracheal tube (8.5 mm cuffed) was inserted. The mean operative time was about 120 min. He was successfully extubated the following day. The postoperative course was uneventful. Daily bronchoscopies and aggressive respiratory physiotherapy were performed to ensure adequate pulmonary toilet. The patient was discharged to a sub-intensive ward ten days after surgery.
Discussion
The reported incidence of tracheobronchial injuries in blunt chest trauma is lower than 5% and, even in large volume Trauma centres, such casualties may be episodical (2,4,10). Kirsh (11) proposed three main theories regarding the mechanism of airway injury in blunt chest trauma. The first theory, or “explosion theory”, involves a rapid increase in airway pressure, especially in the trachea and larger bronchi, while the glottis is still closed. The second approach suggests tracheobronchial disruption with a sudden chest compression, which makes lateral forces pull the lungs apart off the carina. The third theory accounts to a rapid deceleration occurring in high-energy crashes. This mechanism produces a shearing force, causing rupture of the trachea and bronchi. Most of these injuries take place in the distal trachea or the right main bronchus: about 76% occur within 2 cm of the carina (average 1.1 cm) (4,11,12). Right bronchus injuries are more frequently associated with blunt trauma because right bronchus is shorter than the left one, and it supports a bigger and heavier lung, it lies on vertebral bodies that act as an anvil during the impact with less supporting structures than the left bronchus (4,11,12). The last third mechanism most likely produced the bronchial rupture in our report.
In the presence of thoracic trauma and tracheobronchial damage, patient’s conditions can become rapidly fatal, and many of them die directly on the scene of an accident (30–80% in patients with associated lesions of other vital organs) (6,11). In the short term, immediate survival may be possible if transection of the airway is temporarily sealed off by soft tissue. Gasparri et al. (13) analysed admission physiological variables in patients with thoracic trauma: ISS >33±13 was associated with higher mortality. Early diagnosis and treatment are key points in case of tracheobronchial trauma: clinical presentation and CT scans can help the clinicians to recognise this injury. Continuous air leak and persistent pneumothorax should warn the physician. Cassada et al. (9) identified patients with tracheobronchial injuries from their Level 1 Trauma Center Registry during a 10-year period: delay in diagnosis was the only independent prognostic factor for postoperative morbidity (while neither anatomic location nor mechanism of lesion seems to be involved). Timing and delay in shifting the patient to the operating theatre may also play a significant role. Kiser (4), in a review of literature data between 1873 until 1996, reported a median time until diagnosis and surgical treatment of 9 and 25 days, respectively. The median time for diagnosis and surgical treatment of right side injuries was 1 day (mean 161 days) and 3 days (mean 130 days), respectively. In 52% of cases, the diagnosis was made within 24 h for right side injuries. While many patients can be managed non-operatively, a small group requires an emergency thoracotomy. Many authors advocate refractory shock, immediate chest tube output greater than 1,000 mL with persistent bleeding and air leak as indications for immediate surgery. Nishiumi proposed two poor prognostic factors in the case of thoracic trauma associated with lung damage: hemodynamic shock with blood pressure <80 mmHg and heart rate >125 bpm on arrival; more than 1,000 mL of blood lost through the chest tube within 2 h after arrival (6). Damage Control Surgery has been applied to thoracic trauma as well: adequate haemostasis and simpler and quicker procedures such as tractotomy and pneumorrhaphy may be mandatory in patients with underlying coagulopathy, hypothermia or metabolic impairment. In complex chest trauma, lung-sparing surgery should be the target. The resections of lung parenchyma are associated with high mortality; the mortality associated with pneumectomy or massive lobectomy performed for chest trauma can reach 60% (up to 43% for lobectomy, up to 60% for pneumectomy) (4,10-13). Right posterolateral thoracotomy seems the best approach to access lower part of the intrathoracic trachea, the carina, right main stem bronchus and proximal left bronchus (8,12). Also, duration of surgery may influence the outcome of patients with lung injuries. Pneumorrhaphy and pulmonary tractotomy are addressed as a fast way to treat deep pulmonary lacerations. In Gasparri’s (13) retrospective analysis, mean operative time for conservative treatments (tractotomy or pneumorrhaphy) was 196 versus 220 min for resections (lobectomies and pneumonectomies). Also, in Cothren et al. (14) analysis, mean operative time for non-anatomic resections was 135 versus 276 min for anatomical resections: the difference in surgical time between conservative and non-conservative lung techniques for traumatic lesions may also partly explain the difference in mortality. In our case, the operative time was about 120 min.
Non-operative management of these injuries is reserved for patients with isolated small tracheobronchial tears which do not involve the whole thickness of the wall with no respiratory impairment (15). Though non-operative treatment by antibiotics and intubation with the cuff inflated distal to the tear may be effective in some cases, surgical repair is mandatory in many others. Major late morbidity is mostly related to septic complications in intensive care unit, acute respiratory distress syndrome, multiple organ failure and anastomotic dehiscence or stenosis (5,7,9).
Conclusions
Emergency and demolition surgery after extensive blunt chest trauma are associated with high mortality; lung-sparing interventions should be the first choice in these kinds of trauma. Every effort should be made towards conservative surgery to minimise the loss of functional parenchyma, reduce physical impairment and avoid permanent tracheostomy. Unfortunately, most patients are hemodynamically unstable in the ER. Therefore damage control surgery is compulsory. Conservative treatment can be viable only when airway lesions are <2 cm and without hemodynamic or respiratory impairment associated. In many patients, diagnosis of tracheobronchial injury can be delayed to many months after trauma.
In the case described, the patient did not have any other major life-threatening lesions. Therefore it was time to perform a direct repair of the airway with a parenchymal-sparing operation. There are few cases in literature with early diagnosis (about 2 h after trauma), intervention (about 6 h after injury), short surgery time (about 120 min) and rapid extubation (following day) which lead to complete recovery after a blunt chest trauma with a right tracheobronchial damage. Quick decision making and a challenging conservative intervention are the keys to grant a future healthy life.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Before submitting the article, written consent for the publication of this case report was obtained from the patient.
References
- European Commission. Health Statistics. Atlas of mortality in EU: Chapter 5 part 1: Mortality by age; Chapter 20: Violent Deaths. Luxembourg: Office of the Official Publications in EU; 2003. Available online: http://ec.europa.eu/eurostat/en/web/products-statistical-books/-/KS-AC-04-000
- Karmy-Jones R, Wood DE. Traumatic injury to the trachea and bronchus. Thorac Surg Clin 2007;17:35-46. [Crossref] [PubMed]
- Karmy-Jones R, Jurkovich GJ, Shatz DV, et al. Management of traumatic lung injury: a Western Trauma Association Multicenter review. J Trauma 2001;51:1049-53. [Crossref] [PubMed]
- Kiser AC, O'Brien SM, Detterbeck FC. Blunt tracheobronchial injuries: treatment and outcomes. Ann Thorac Surg 2001;71:2059-65. [Crossref] [PubMed]
- Richardson JD. Outcome of tracheobronchial injuries: a long-term perspective. J Trauma 2004;56:30-6. [Crossref] [PubMed]
- Nishiumi N, Inokuchi S, Oiwa K, et al. Diagnosis and treatment of deep pulmonary laceration with intrathoracic hemorrhage from blunt trauma. Ann Thorac Surg 2010;89:232-8. [Crossref] [PubMed]
- Rossbach MM, Johnson SB, Gomez MA, et al. Management of major tracheobronchial injuries: a 28-year experience. Ann Thorac Surg 1998;65:182-6. [Crossref] [PubMed]
- Gabor S, Renner H, Pinter H, et al. Indications for surgery in tracheobronchial ruptures. Eur J Cardiothorac Surg 2001;20:399-404. [Crossref] [PubMed]
- Cassada DC, Munyikwa MP, Moniz MP, et al. Acute injuries of the trachea and major bronchi: importance of early diagnosis. Ann Thorac Surg 2000;69:1563-7. [Crossref] [PubMed]
- Kummer C, Netto FS, Rizoli S, et al. A review of traumatic airway injuries: potential implications for airway assessment and management. Injury 2007;38:27-33. [Crossref] [PubMed]
- Kirsh MM, Orringer MB, Behrendt DM, et al. Management of tracheobronchial disruption secondary to nonpenetrating trauma. Ann Thorac Surg 1976;22:93-101. [Crossref] [PubMed]
- Mussi A, Ambrogi MC, Ribechini A, et al. Acute major airway injuries: clinical features and management. Eur J Cardiothorac Surg 2001;20:46-51, discussion 51-2. [Crossref] [PubMed]
- Gasparri M, Karmy-Jones R, Kralovich KA, et al. Pulmonary tractotomy versus lung resection: viable options in penetrating lung injury. J Trauma 2001;51:1092-5; discussion 1096-7. [Crossref] [PubMed]
- Cothren C, Moore EE, Biffl WL, et al. Lung-sparing techniques are associated with improved outcome compared with anatomic resection for severe lung injuries. J Trauma 2002;53:483-7. [Crossref] [PubMed]
- Martin MJ, McDonald JM, Mullenix PS, et al. Operative management and outcomes of traumatic lung resection. J Am Coll Surg 2006;203:336-44. [Crossref] [PubMed]
Cite this article as: Scognamiglio G, Solli P, Benni M, Davoli F, Pardolesi A, Bertolaccini L, Agnoletti V. Less is more: lung-sparing direct repair of a traumatic rupture of the bronchus intermedius. J Vis Surg 2017;3:109.