VATS hand sewn intrathoracic esophagogastric anastomosis
Introduction
Totally endoscopic two stage (laparoscopic and VATS) esophagectomy for carcinoma of the lower third esophagus is a well-established procedure (1,2). There are currently many methods to perform the intrathoracic esophagogastric anastomosis by VATS (3). The technique described here is an extension of the same technique used by the first author for VATS right upper lobe sleeve lobectomy for lung cancer (4). Using the same VATS sleeve upper lobectomy incisions and technique the hand sewn intrathoracic esophagogastric anastomosis can be performed in a safe and simple way, replicable by most experienced VATS surgeon.
Methods
Clinical summary
Patient
A 64-year-old male with a T2N0M0 adenocarcinoma of the lower third of the esophagus. EUS/OGD showed a T2 cancer 35 cm from the incisions. PET CT showed no evidence of lymph node or distant metastasis.
Technique
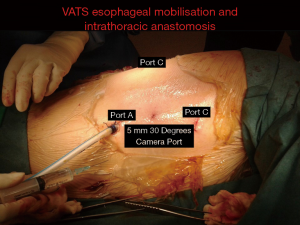
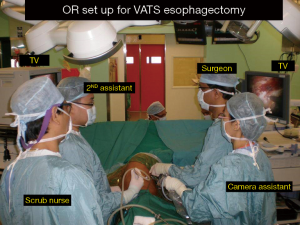
The patient underwent a totally laparoscopic mobilization of the stomach conduit based on the left gastroepiploic vessels. Once the abdominal phase of the surgery was completed the patient was turned to the left lateral decubitus position for the thoracic part. The right lung was isolated with a left double lumen endotracheal tube. Three incisions were made. A 5-mm camera port at the mid axillary line 5th intercostal space, followed by a 10-mm working port at the 6th intercostal space posterior axillary line and a 2-cm utility incision at the 3rd intercostal spaces anterior axillary line respectively (Figure 1, ports A and B). An optional 5-mm retraction post can be placed at the 6th intercostal space inferior and posterior to the scapular tip. (port C, Figure 1) if needed. The surgeon and the camera assistant stand in front of the patient as in an anterior approach in VATS lobectomy (Figure 2). The operating table is then rotated anteriorly towards the surgeon to a semi-prone position to allow the lung to fall away from the operative field under gravity (Figure 3).
After opening the mediastinal pleura the azygos vein is stapled and divided with a vascular stapler. Mediastinal lymphadenectomy is completed and the esophagus is then encircled with a tape for retraction. The esophagus is then mobilized proximally and distally. The periesophageal hiatal attachments are then divided and the gastric conduit is the delivered into the chest. The proximal esophagus and the distal gastric junction are then divided with endostaplers at an appropriate level from the tumour for safe margins. The specimen is then removed in an endobag by enlarging the cranial most 10-mm port. Once the margins are confirmed to be negative for malignancy on frozen section the anastomosis is then performed after ensuring there is no torsion with proper alignment of the conduit and esophagus (Figure 4).

The anastomosis is done high up in the chest at the thoracic inlet to prevent conduit redundancy and reflux. The posterior wall of the proximal esophagus is tagged to the stomach with interrupted seromuscular sutures with polydiaxone (PDS) 4 0. The esophageal muscle layer is then divided first followed by the mucosal layer. This prevents retraction of the mucosal layer and ensures an accurate mucosal to mucosal anastomosis. The stomach is then opened. An end to end esophagogastric anastomosis is done with interrupted 40 PDS sutures starting in the center and working towards both ends. The sewing is done with a 5-mm endo-needle holder through the port B. This port is ergonomically ideal for sewing the anastomosis as the needle holder and the direction of sewing is 90 degrees perpendicular to the esophagus and stomach anastomotic openings (Figure 5), Once the posterior ends are completed Connell stitches are inserted at both ends to ensure inversion and accurate mucosal apposition when doing the anterior layer. The nasogastric tube is then passed through the anastomosis and the anterior layer is completed with similar interrupted sutures. The last few anterior all sutures are preplaced before tying. Tissue glue is applied over the anastomosis and a size 24 F chest tube is placed (Figure 6).


Post-operative management and outcome
The patient made an uneventful recovery. Oral contrast swallow study on 7th post-operative day showed no evidence of leak with free flow of contrast into the small bowel. Final pathology shows a T2N1M0 adenocarcinoma of the lower esophagus with clear surgical margins but two perigastric lymph nodes were positive for malignancy. Patient was referred for adjuvant chemotherapy.
Conclusions
Since 2014 we have performed this technique on nine patients with no leak or strictures to date. Totally hand sewn intrathoracic esophagogastric anastomosis is a safe, replicable and simplified technique which can be easily performed by most experienced VATS/laparoscopic surgeons. It allows for an accurate and wide mucosal to mucosal anastomosis between the esophagus and the stomach high up in the thoracic inlet with safe oncological margins.
Preference card
- 5-mm 30 degrees camera;
- 5-mm endoscopic needle holder;
- 4-0 PDS sutures;
- 5-mm endoscopic knot pusher.
Tricks and pitfalls
- The first layer of seromuscular anchoring sutures between the posterior wall of esophagus and stomach are important in taking away tension on the anastomosis and for proper alignment of the anastomosis without tension;
- It is important to perform a circumferential myotomy on the esophagus first and then to cut the mucosal layer longer. This ensures the mucosal layer is longer than the muscle layer and prevents retraction of the mucosa into the esophagus and allowing for accurate mucosal to mucosal anastomosis;
- The corner Connell sutures are important in inverting the mucosal layer before performing the anterior anastomosis;
- Mandatory to put port C in the 3rd intercostal space. This gives a direct perpendicular access to sewing of both ends. Removing the specimen by enlarging this incision facilitates sewing and tying.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [Crossref] [PubMed]
- Palanivelu C, Prakash A, Senthilkumar R, et al. Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position--experience of 130 patients. J Am Coll Surg 2006;203:7-16. [Crossref] [PubMed]
- Blackmon SH, Correa AM, Wynn B, et al. Propensity-matched analysis of three techniques for intrathoracic esophagogastric anastomosis. Ann Thorac Surg 2007;83:1805-13; discussion 1813.
- Agasthian T. Initial experience with video-assisted thoracoscopic bronchoplasty. Eur J Cardiothorac Surg 2013;44:616-23. [Crossref] [PubMed]
- Agasthian T, Shabbir A. VATS mobilization of thoracic esophagus. Asvide 2017;4:266. Available online: http://www.asvide.com/articles/1575
- Agasthian T, Shabbir A. Outside operative view of VATS intrathoracic anastomosis. Asvide 2017;4:267. Available online: http://www.asvide.com/articles/1576
- Agasthian T, Shabbir A. VATS intrathoracic handsewn esophagogastric anastomosis. Asvide 2017;4:268. Available online: http://www.asvide.com/articles/1577
Cite this article as: Agasthian T, Shabbir A. VATS hand sewn intrathoracic esophagogastric anastomosis. J Vis Surg 2017;3:90.