Three-dimensional video-assisted thoracic surgery for pulmonary resections: an update
Introduction
Video-assisted thoracic surgery (VATS) is performed to treat non-small cell lung cancer, metastatic disease, benign tumors and mediastinal neoplasms. Compared with thoracotomy, VATS enables a smaller incision without stretching of the ribs avoiding injuries to respiratory muscles and minimizing postoperative lung function impairment. Moreover, with a thoracoscopic access, patients experience less postoperative pain and expectorate more easily, thus reducing the incidence of pulmonary infection and other complications (1). Since the early 1990s (2,3), traditional two-dimensional (2D) VATS has rapidly developed and has been widely applied around the world. However, a 2D image lacks depth resulting in image distortion, impaired hand-eye coordination and decreased ability to estimate size and to assess spatial orientation. Moreover, as reported by Pardolesi et al. (4), 2D VATS encloses other disadvantages such as poorer visualization of the structures of the hilum resulting in a difficulty in dissection of the planes. The visual information gained via binocular vision allows for precise intraoperative movement and can therefore affect surgical procedure (5), though surgeons try to compensate for these limitations by using 2D cues such as light and shade, relative size of organs, organ interposition, texture gradient, aerial perspective and motion parallax (6). Some of these aspects have been corrected with the introduction of robot-assisted thoracic surgery (RATS), characterized by 3D magnified visualization, high degrees of freedom and by oncological outcomes comparable both with thoracotomy and VATS (7,8). On the other hand, major issues derive from health costs and profits, in particular rapid depreciation of capital combined with robot-specific equipment costs (9). With the introduction of 3D VATS, the advantages of VATS and robotic surgery were potentially combined. Although depth perception has significantly improved since the early experiences with 3D endoscopic surgery, headaches and ocular fatigue during the procedure claimed urgent technical adjustments (10). Now, 3D minimally-invasive approach can be performed stereoscopically by wearing 3D glasses. Despite the significant advantages, it is unclear whether 3D VATS is superior to the 2D VATS systems.
The aim of the study is to perform a comprehensive review of literature on the 3D method in thoracic surgery and to assess its feasibility in parenchymal resection according to recent published data.
Surgical technique considerations (Figures 1,2)


3D VATS combines aspects of both 2D VATS and RATS. A 3D optics with a 100-degree angulating endoscope with high range of motion allows a proper visualization of the hilum, some surgical threatening areas (i.e., Boyden’s trunk, right upper paratracheal space and Le Brigand’s intrapulmonary vascular cross) and anatomic dissection planes (i.e., fissures, posterior mediastinum). 3D spectacles are part of the equipment and worn by all personnel. Hardware are similar to 2D technology ones and composed by light sources, carbon dioxide insufflation systems, screens and HD-hard disk drives in order to record procedures simultaneously in both 2D and 3D. Moreover, glasses are interchangeable and visualization is undisturbed through them during the beginning of the surgical procedure (i.e., port placement, skin incisions), resulting in reduced frequency of visual disturbances, headache, spatial disorientation. We usually use the Karl Storz (KARL STORZ GmbH & Co. KG, Tuttlingen, Deutschland) equipment consisting of: (I) 10 mm, 0-degree and 30-degree viewing angle 3D Video Thoracoscope TIPCAM Spies with 3D fiber optic cable; (II) Image 3D Link module, for connecting the Video Thoracoscope; (III) 3D 32’’ Monitor; (IV) AIDA Recording System; (V) Basket for 3D optical sterilization; (VI) 3D Glasses. The attached shows a 3D VATS right lower lobectomy for lung cancer. 3D imaging improves depth perception, spatial location and precision of the surgical performance especially during advanced technical maneuvers (13,14). The correctional moves enhancement allows a higher degree of accuracy during grasping thanks to its dual optics technology, brighter focus-free images, reduced fogging and a viewing angle without loss of visual horizon or orientation (15). Concerning the first aspect, Sahu et al. (16) reported accuracy in spatial perception allowing an excellent hand-eye coordination and leading to an accurate and swift dissection. These authors also affirmed that 3D HD system offers many advantages of robotic surgery at low cost and with the use of conventional laparoscopic equipment. They stated that advantages of 3D laparoscopy were well appreciated in training models as well as during operative procedures. Furthermore, surgical technique is the same in 3D when compared with 2D VATS and thus no new learning curve for an experienced VAT surgeon is required (which indeed is the case with robotic surgery). These distinctive features are mainly attributable to the presence of the same surgical movements, of a “filtered” tactile sensitivity (RATS lacks of tactile feedback) and the adoption of the same surgical access. For trainees or surgeons without any experience on video-assisted surgery, the learning curve will be shorter and less steep because no adaptation to 2D and visualization depth-related tricks are required. The angulation of the tip of the camera to a maximum of 100 degrees facilitates major vessels dissection and linear staplers positioning. These advantages should result, as demonstrated in randomized studies in laparoscopic surgery, both in an improved learning curve and shorten task performance times in novice trainees as well as experienced surgeons (17,18). With concerns to robotic pulmonary resections, RATS is more ergonomic than 3D VATS due to its in-line-axis with surgeon controller, position (head- and arm-support), excellent 3D view and a superb 360-degree of range of motion for all instruments (dissectors and staplers) (4). However, the 3D VATS technique has a comparable view on the operation field, plus the advantage of the flexible camera tip which enables the looking-around-the-corner-view.
2D vs. 3D VATS
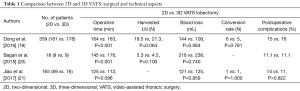
As an emerging imaging system and technique, 3D VATS is an interesting resource for thoracic surgeons. However, limited data have been published on clinical experiences with 3D compared to 2D devices. Dong et al. (19), in a large retrospective study on 359 non-small cell lung cancer patients, compared surgical outcomes and perioperative follow up according to the minimally invasive strategy adopted (181 2D vs. 178 3D VATS patients) by matching them for age, tumor size and location. Concerning mean operative time between the aforesaid groups (3D vs. 2D), a significant statistical difference was found (163 vs. 184 min, P<0.001). On the other hand, no differences according to the mean number of harvested lymph nodes, the intraoperative estimated volume of blood loss, conversion rates and major postoperative complications were found (21.3 vs. 19.5, P=0.064; 109 vs. 144 mL, P=0.064; 5 vs. 6, P=0.781; and 16% vs. 15%, respectively). Similar results have been reported by Bagan et al. (20) in 18 patients undergoing 3D thoracic surgery. Authors found a significant reduction of surgical time in 3D brace (145 vs. 176 min, P<0.001) but the tube duration, number of lymph node stations and upstaging were similar between the groups. Finally, Jiao et al. (21) recently investigated 165 patients (76 3D and 89 2D) who underwent pulmonary lobectomy and systematic dissection of mediastinal lymph nodes for lung cancer. No statistical difference was found between the two groups with respect to duration of surgery, volume of intraoperative bleeding, drainage volume after surgery, duration of drainage tube insertion, hospitalization time after surgery, hospitalization costs and complications (P>0.05). Additionally, there was no significant difference in the numbers and groups of all lymph nodes or N2 lymph nodes resected (P>0.05). Authors concluded pulmonary lobectomy could be undertaken with two ports using a 3D method with similar results than 2D group with no greater hospitalization costs but with better operational perception and sensitivity during surgery (Table 1). Concerning these early experiences, 3D system advantages seem to lie in a significant reduction of operative time, similar to those published for laparoscopy (18). These benefits derive from the better depth visualization of 3D technology, not to be achieved with traditional 2D without an increase in visual strain for surgeons. Subsequently, this influences both intraoperative complication (22) and conversion rates (23).
Full table
3D VATS vs. RATS
3D technology is shared both by 3D VATS and RATS. Robotic surgery rationale lies on a telerobotic system with a true 3D endoscope providing high-resolution binocular view of the surgical procedure (24). The “da Vinci system” has been applied to an increased number of thoracic surgical procedures (25-28) and in particular to pulmonary lobectomies (29-31); however, no data comparing robotic with 3D assisted lobectomy are published at this date.
Telerobotics improved dexterity by an active filtration of surgeon tremors, with ergonomic advantages, such as its in-line-axis controller, its head- and arm-support reducing fatigue and the excellent 3D view and a superb 360-degree of range of motion for all instruments (dissectors and staplers) (32). However, the drawback of the “da Vinci system” is the high costs both in implementation and maintenance and in the rapid depreciation of instrumentation, lack of tactile feedback to the surgeon, the bulk of the robotic arms in the operation room leading to time delay (33). For these reasons, robotic technology and surgery is currently far from universal, except for urological and gynecological operations (34,35). In this setting, 3D HD systems may be an effective intermediate solution between traditional 2D laparoscopic and thoracoscopic surgery and RATS, due to the combination of minimally invasiveness, low costs and high standards in technical resources (i.e., 3D looking-around-the-corner-view), making them accessible even to developing countries.
Health costs analysis
Yang et al. (36) reported an extensive and detailed care costs analysis by comparing 2D and 3D VATS lobectomy in 3,000 NSCLC patients. Indirect expenses such as salaries, insurances, utilities and building depreciation were excluded due to similarity between groups. On the other hand, direct hospital cost data were collected and clustered into distinct categories such as operating room, intensive care unit, staplers and surgical supplies. Authors concluded there were no statistically significant differences both in each cost category and total cost [11,486.73 vs. 11,388.21 USD (10,844.62 vs. 10,751.61 EUR), P=0.913]. The same conclusions were reported by Jiao et al. (21) referring to VATS lobectomy [59,900 vs. 58,900 CNY (8,689.45 vs. 8,544.38 USD or 8,196.05 vs. 8,059.22 EUR), P=0.207]. This can be important from a hospital and health system point-of-view in the current era of reducing expenses on health-care; the higher cost of robotic surgery deriving from instrumentation and a lower profit to system depreciation ratio might be a reason to adapt the 3D technique rather than the robotic technique one. These differences will be probably re-discussed only at the forthcoming “da Vinci system” patent expiry. Deen et al. (9), in a fascinating review on health economics reporting 184 consecutive lung cancer patients, showed no statistically significant difference in overall cost between VATS and open cases (Δ =$1,207) or open and robotic cases (Δ =$1,975); but, robotics burdened $3,182 more than VATS (P<0.001) owing to robotic-specific supplies costs. Authors stated that the main opportunities to reduce cost in thoracotomy cases were the intensive care unit, respiratory therapy and laboratories. On the other hand, minimally invasive thoracic surgery claimed a strict reduction of operating times and supply costs to be competitive.
Conclusions
With advances in 3D technology, high-definition imaging systems now provide significantly improved picture quality and resolution, similar to the robotic one. Several studies have shown the advantages of 3D HD over conventional 2D HD in terms of improving surgeon performance in standardized basic skills tasks. The integration of 3D systems has improved minimally-invasive thoracic strategies and in the field of endoscopically assisted oncological surgery. An efficient 3D device increases surgical outcomes in a shorter time. Surely, another aspect to consider is the wide accessibility of the technology itself especially to developing countries. In an era of drastic cuts in health care costs, 3D is definitely more attractive than the much more expensive robotic technology. However, 3D results need to be confirmed and compared in a larger, prospective and multi-institutional databases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Roviaro G, Varoli F, Rebuffat C, et al. Videothoracoscopic staging and treatment of lung cancer. Ann Thorac Surg 1995;59:971-4. [Crossref] [PubMed]
- Roviaro G, Rebuffat C, Varoli F, et al. Videothoracoscopic excision of mediastinal masses: indications and technique. Ann Thorac Surg 1994;58:1679-83; discussion 1683-4.
- Pardolesi A, Park B, Petrella F, et al. Robotic anatomic segmentectomy of the lung: technical aspects and initial results. Ann Thorac Surg 2012;94:929-34. [Crossref] [PubMed]
- Chan AC, Chung SC, Yim AP, et al. Comparison of two-dimensional vs three-dimensional camera systems in laparoscopic surgery. Surg Endosc 1997;11:438-40. [Crossref] [PubMed]
- Storz P, Buess GF, Kunert W, et al. 3D HD versus 2D HD: surgical task efficiency in standardised phantom tasks. Surg Endosc 2012;26:1454-60. [Crossref] [PubMed]
- Farivar AS, Cerfolio RJ, Vallières E, et al. Comparing robotic lung resection with thoracotomy and video-assisted thoracoscopic surgery cases entered into the Society of Thoracic Surgeons database. Innovations (Phila) 2014;9:10-5. [Crossref] [PubMed]
- Park BJ, Melfi F, Mussi A, et al. Robotic lobectomy for non-small cell lung cancer (NSCLC): long-term oncologic results. J Thorac Cardiovasc Surg 2012;143:383-9. [Crossref] [PubMed]
- Deen SA, Wilson JL, Wilshire CL, et al. Defining the cost of care for lobectomy and segmentectomy: a comparison of open, video-assisted thoracoscopic, and robotic approaches. Ann Thorac Surg 2014;97:1000-7. [Crossref] [PubMed]
- Hanna GB, Shimi SM, Cuschieri A. Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 1998;351:248-51. [Crossref] [PubMed]
- Divisi D, Barone M, Crisci R. Right lower lobectomy in 2D VATS. Asvide 2017;4:232. Available online: http://www.asvide.com/articles/1541
- Divisi D, Barone M, Crisci R. Right lower lobectomy in 3D VATS. Asvide 2017;4:233. Available online: http://www.asvide.com/articles/1542
- Lusch A, Bucur PL, Menhadji AD, et al. Evaluation of the impact of three-dimensional vision on laparoscopic performance. J Endourol 2014;28:261-6. [Crossref] [PubMed]
- Votanopoulos K, Brunicardi FC, Thornby J, et al. Impact of three-dimensional vision in laparoscopic training. World J Surg 2008;32:110-8. [Crossref] [PubMed]
- Kunert W, Storz P, Kirschniak A. For 3D laparoscopy: a step toward advanced surgical navigation: how to get maximum benefit from 3D vision. Surg Endosc 2013;27:696-9. [Crossref] [PubMed]
- Sahu D, Mathew MJ, Reddy PK. 3D Laparoscopy - Help or Hype; Initial Experience of A Tertiary Health Centre. J Clin Diagn Res 2014;8:NC01-3. [PubMed]
- Tanagho YS, Andriole GL, Paradis AG, et al. 2D versus 3D visualization: impact on laparoscopic proficiency using the fundamentals of laparoscopic surgery skill set. J Laparoendosc Adv Surg Tech A 2012;22:865-70. [Crossref] [PubMed]
- Wilhelm D, Reiser S, Kohn N, et al. Comparative evaluation of HD 2D/3D laparoscopic monitors and benchmarking to a theoretically ideal 3D pseudodisplay: even well-experienced laparoscopists perform better with 3D. Surg Endosc 2014;28:2387-97. [Crossref] [PubMed]
- Dong S, Yang XN, Zhong WZ, et al. Comparison of three-dimensional and two-dimensional visualization in video-assisted thoracoscopic lobectomy. Thorac Cancer 2016;7:530-534. [Crossref] [PubMed]
- Bagan P, De Dominicis F, Hernigou J, et al. Complete thoracoscopic lobectomy for cancer: comparative study of three-dimensional high-definition with two-dimensional high-definition video systems. Interact Cardiovasc Thorac Surg 2015;20:820-3. [Crossref] [PubMed]
- Jiao P, Wu QJ, Sun YG, et al. Comparative study of three-dimensional versus two-dimensional video-assisted thoracoscopic two-port lobectomy. Thorac Cancer 2017;8:3-7. [Crossref] [PubMed]
- Velayutham V, Fuks D, Nomi T, et al. 3D visualization reduces operating time when compared to high-definition 2D in laparoscopic liver resection: a case-matched study. Surg Endosc 2016;30:147-53. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Ballantyne GH. Robotic surgery, telerobotic surgery, telepresence, and telementoring. Review of early clinical results. Surg Endosc 2002;16:1389-402. [Crossref] [PubMed]
- Mussi A, Fanucchi O, Davini F, et al. Robotic extended thymectomy for early-stage thymomas. Eur J Cardiothorac Surg 2012;41:e43-6; discussion e47.
- Ward AF, Lee T, Ogilvie JB, et al. Robot-assisted complete thymectomy for mediastinal ectopic parathyroid adenomas in primary hyperparathyroidism. J Robot Surg 2017;11:163-9. [PubMed]
- Willems E, Martens S, Beelen R. Robotically enhanced mediastinal teratoma resection: a case report and review of the literature. Acta Chir Belg 2016;116:309-312. [Crossref] [PubMed]
- Chiu PW, Teoh AY, Wong VW, et al. Robotic-assisted minimally invasive esophagectomy for treatment of esophageal carcinoma. J Robot Surg 2017;11:193-9. [PubMed]
- Kocher GJ, Schmid RA, Melfi FM. Robotic lobectomy: tips, pitfalls and troubleshooting. Eur J Cardiothorac Surg 2014;46:e136-8. [Crossref] [PubMed]
- Ambrogi MC, Fanucchi O, Melfi F, et al. Robotic surgery for lung cancer. Korean J Thorac Cardiovasc Surg 2014;47:201-10. [Crossref] [PubMed]
- Veronesi G, Agoglia BG, Melfi F, et al. Experience with robotic lobectomy for lung cancer. Innovations (Phila) 2011;6:355-60. [Crossref] [PubMed]
- Nezhat C, Lewis M, Kotikela S, et al. Robotic versus standard laparoscopy for the treatment of endometriosis. Fertil Steril 2010;94:2758-60. [Crossref] [PubMed]
- Bodner JC, Zitt M, Ott H, et al. Robotic-assisted thoracoscopic surgery (RATS) for benign and malignant esophageal tumors. Ann Thorac Surg 2005;80:1202-6. [Crossref] [PubMed]
- Hu JC, O'Malley P, Chughtai B, et al. Comparative Effectiveness of Cancer Control and Survival after Robot-Assisted versus Open Radical Prostatectomy. J Urol 2017;197:115-21. [Crossref] [PubMed]
- Bodur S, Dede M, Firatligil FB, et al. A Cost-Effective Approach in Gynecologic Robotic Surgery. J Minim Invasive Gynecol 2015;22:S68-S69. [Crossref] [PubMed]
- Yang C, Mo L, Ma Y, et al. A comparative analysis of lung cancer patients treated with lobectomy via three-dimensional video-assisted thoracoscopic surgery versus two-dimensional resection. J Thorac Dis 2015;7:1798-805. [PubMed]
Cite this article as: Divisi D, Barone M, Crisci R. Three-dimensional video-assisted thoracic surgery for pulmonary resections: an update. J Vis Surg 2017;3:79.


