Intra-pericardial double sleeve uniportal video-assisted thoracoscopic surgery left upper lobectomy
Introduction
Sleeve resections for lung cancer are indicated for tumors involving the proximal part of lobar bronchus or artery, but with limited infiltration where pneumonectomy could be avoided and R0 resection can be achieved. Sleeve resection surgeries can provide better long-term survival than Pneumonectomy, with no increase of postoperative complications or recurrence rate (1-3). Despite the complexity of double sleeve lobectomy operations, recent reports describing the technique and safety of this procedure were published recently by video-assisted thoracoscopic surgery (VATS) experts using 1–4 incisions (4-8). VATS surgery did have its’ learning curve for the surgeon and the assistant. Based on our experience in uniportal and multi-portal VATS in a very high volume center we performed a case of Intra-pericardial double sleeve left upper lobectomy for non-small cell lung cancer we herein describe our technique in performing this procedure.
Patient and workup
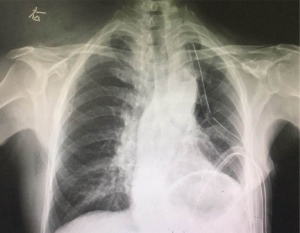
A 66 years old, male, heavy smoker patient presented to our clinic with complains of worsening dry cough for the last six months, CT scan revealed a 5 cm hilar mass in the left lung invading the pulmonary artery and the left bronchus (Figure 1). Bronchoscopy (Figure 2) and transbronchial biopsy was performed and revealed a diagnosis of squamous cell carcinoma. EBUS revealed no lymph nodes involvement. Thus a decision was made to resect the tumor via the intercostal uniportal approach.
Pre-operative preparations
The operation was scheduled to be performed with intercostal uniportal VATS technique. The patient was intubated with a double lumen endotracheal tube (39 Fr), CVP line, arterial line, and urinary catheters were inserted before beginning of the surgery.
Equipment performance card
Full HD thoracoscopic camera (Karl Storz®), vascular tourniquet and wound protector (Changzhou Company Ltd.), special instruments designed for VATS surgery (Shanghai Medical Instruments Group Ltd.), TA ™staplers (Covedien-Medtronic), and PROLENE® sutures.
Procedure
Under general anesthesia, insertion of venous access lines, arterial line and urinary catheter. The patient positioned on right decubitus position, bronchoscopy was performed and revealed a tumor that protruding from the bronchus of the upper lobe to the lumen of main bronchus. 3.5 cm intercostal incision was performed at the anterior axillary line of the fourth intercostal space. Pleural adhesions were removed using cautery (Figure 3). The pericardium was opened longitudinally just above the main pulmonary artery and left superior pulmonary vein posterior to the phrenic nerve. After dissecting and encircling the left main pulmonary artery and the left superior pulmonary vein the ligamentum arteriosum was transected in order to provide wider space around the left main pulmonary artery. After infusing 5,000 units of intra-venous Heparin, proximal control of the artery was achieved using a vascular tourniquet. The next step was developing the inter-lobar fissure which was not involved by the tumor. The interlobar artery was exposed and the segment branch to the left upper posterior segment (S2) was tied using silk tie and transected using energy device (LigaSure™). Distal arterial control was subsequently achieved by encircling the left lower lobe superior and basal segmental arteries, which were occluded separately by two vascular tourniquets. Subsequently, the left superior pulmonary vein was stapled as well using TA™ stapler. After that the left main pulmonary artery was transected with scissors proximal and distal to the tumor invasion area (vascular sleeve), and the Left superior pulmonary vein was transected above the stapler line using scissors. Next step was dissecting the left main bronchus and its upper lobe branch, which was transected using scissors and the specimen was removed from the chest cavity using a retrieval bag. The transection of the left main bronchus then was completed (bronchial sleeve resection), and the subcarinal lymph nodes were removed. The double sleeve reconstructive anastomoses then were started first by the bronchial anastomosis using running non-absorbable two needles sutures (PROLENE® 3/0). We started the anastomosis from the posterior wall of the bronchus toward the anterior cartilaginous part. By the end of anastomosis, the knot was placed outside the bronchial lumen. The lower lobe then was inflated, and the competency of the anastomosis was checked. The adventitia of the aortic arch was dissected in order to create a flap which was sewn over the bronchial anastomosis for protection of the anastomosis and to separate it from the vascular anastomosis. Next step was to perform the arterial sleeve anastomosis which was performed using non-absorbable two needles (PROLENE® 5/0) suture with the same technique described before for the bronchial anastomosis starting from the medial arterial wall and ending at the lateral wall. Before knotting the anastomosis de-airing of the artery was done by releasing the distal tourniquet. Then the anastomosis was completed by knotting the suture using a knot pusher. No bleeding was noticed after removing the proximal tourniquet. After hemostasis, a single chest drain was inserted through the same incision, frozen section confirmed that all the surgical margins were free of tumor cells, total surgical time was (290 minutes) and estimated blood loss was (200 cc).
Post-operative management
Post-operative course was uneventful. Post-operative radiographic X-ray showed a fully expanded lungs without residual air or fluid (Figure 4). Chest drain was removed in POD (3), and the patient was discharged in POD (4). Final diagnosis was T4N0M0 squamous cell carcinoma of lung.
Tips, tricks and pitfalls
- Opening the pericardium in central tumors and sleeve resections can provide wider space for stapling and control of the vessels;
- Transect the aorto-pulmonary ligament provide wider space for applying the vascular tourniquet around the pulmonary artery and facilitates the anastomosis;
- Wrapping the vascular anastomosis with aortic adventitia flap is a good option as it’s vascularized non-foreign tissue that can protect the anastomosis and prevent fistula formation;
- Placement of tourniquet inside the pleural space during the surgery in the way that demonstrated in the video (Figure 5) can provide better space for instrumentation through a single incision.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Maurizi G, D'Andrilli A, Anile M, et al. Sleeve lobectomy compared with pneumonectomy after induction therapy for non-small-cell lung cancer. J Thorac Oncol 2013;8:637-43. [Crossref] [PubMed]
- Ma Z, Dong A, Fan J, et al. Does sleeve lobectomy concomitant with or without pulmonary artery reconstruction (double sleeve) have favorable results for non-small cell lung cancer compared with pneumonectomy? A meta-analysis. Eur J Cardiothorac Surg 2007;32:20-8. [Crossref] [PubMed]
- Gaissert HA, Mathisen DJ, Moncure AC, et al. Survival and function after sleeve lobectomy for lung cancer. J Thorac Cardiovasc Surg 1996;111:948-53. [Crossref] [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Liu L, Mei J, Pu Q, et al. Thoracoscopic bronchovascular double sleeve lobectomy for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;46:493-5. [Crossref] [PubMed]
- Han Y, Zhou S, Yu D, et al. Video-assisted thoracic surgery (VATS) left upper sleeve lobectomy with partial pulmonary artery resection. J Thorac Dis 2013;5 Suppl 3:S301-3. [PubMed]
- Hennon M, Sahai RK, Yendamuri S, et al. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol 2011;18:3732-6. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, Fieira E, et al. Uniportal video-assisted thoracoscopic bronchial sleeve lobectomy: first report. J Thorac Cardiovasc Surg 2013;145:1676-7. [Crossref] [PubMed]
- Abu Akar FE, Yang C, Lin L, et al. Intra-pericardial double sleeve uniportal video-assisted thoracoscopic surgery (VATS) left upper lobectomy. Asvide 2017;4:139. Available online: http://www.asvide.com/articles/1447
- Abu Akar FE, Yang C, Lin L, et al. Technique of placement and securing the vascular control tourniquet. Asvide 2017;4:140. Available online: http://www.asvide.com/articles/1448
Cite this article as: Abu Akar F, Yang C, Lin L, Min SJ, Jiang L. Intra-pericardial double sleeve uniportal video-assisted thoracoscopic surgery left upper lobectomy. J Vis Surg 2017;3:51.