The Athens uniportal video-assisted thoracic surgery masterclass—an ambitious kickstarter
The history of modern thoracic surgery has been demarcated by the dramatic shift from open surgery to minimally invasive techniques. Certain advancements in camera technology and surgical instruments have augmented this shift (1). However, the evolution is a constant and dynamic process. Video assisted thoracic surgery has further evolved from multiport techniques to the uniportal or single incision technique. The latter is rapidly gaining popularity as the concept of conducting major thoracic operations through a single incision is appealing indeed.
The uniportal technique was initially described for diagnostic purposes more than a decade ago (2). However only after a successful single port lobectomy was reported 6 years ago, did it draw the attention of the thoracic community (3). Owing to it being even less invasive, with favourable geometric characteristics that enhance the view of the surgical target (4), the uniportal approach has emerged as the most recent and promising evolution of VATS. Studies have already been published demonstrating the technique’s feasibility, safety and oncologic efficacy not only for early stage lung cancer, but also for more advanced cases and complex procedures (5,6). Its impact spreads across the thoracic domain, calling for even less invasiveness, not only surgical but also anaesthetic. The industry, is now taking into consideration the single port access challenges. Instrument design and development has become more sophisticated; long and low profile shafts, double articulation, specific angulation are all aspects of modern surgical tools designed to overcome them. Robotic arm prototypes incorporate into a single shaft a camera and two or more instruments.
The significant and rapid spread of the uniportal technique may be attributed to the fact that it closely resembles the anterior approach achieved by an anterolateral thoracotomy. Surgeons familiar with the latter, may progress to single incision VATS without previous advanced VATS experience. In addition, placing the camera at the uppermost part of the incision and above the surgeon’s instruments produces an accurate enough imitation of the “eyes above hands” sense of vision, possibly facilitating the eye—hands coordination, an issue surgeons may face when starting VATS. However, the task to manoeuvre two or three instruments via a single incision, part of which is occupied by the scope, can be challenging without the appropriate instrumentation.
The fast adoption of the technique introduces a need for the establishment of an organized, periodical and structured training program, which will set the standards of the technique and ensure that the trainees will acquire the essential theoretical knowledge before starting. Such a program has been running for more than 2 years now, at the Shanghai Pulmonary Hospital.
In Hellas, apart from ours, two institutions have reported on their minimally invasive lobectomy series. In our institution, the uniportal technique is the standard approach for almost any thoracic procedure, excluding esophageal and mesothelioma surgery. The technique was first implemented following the author’s visit at the Shanghai Pulmonary Hospital in October 2014. Since then, significant experience has been gained, leading to the announcement of our department’s series of uniportal lobectomies during the 11th PanHellenic Cardiothoracic Conference, in November 2016.
With the organisation of the Athens Uniportal VATS master class by our department last December, an educational cycle was completed. The Hellenic thoracic community had the opportunity to attend a 2-day intensive tutorial on the technique by Dr. Rivas, which was climaxed by live surgery on the second day. The topics outlined during the master class are presented on Table 1. The cases operated on during the second day are briefly presented below.
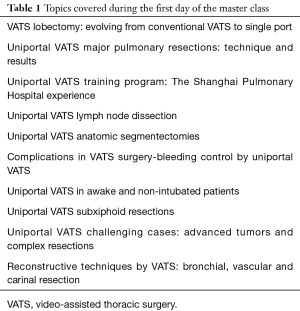
Full table
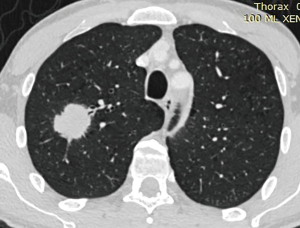
Case 1
A 45 years old male, active smoker, who was incidentally diagnosed with a 3.1 cm, PET-CT positive, solid mass on the right upper lobe, following a chest X-ray for lower respiratory tract infection (Figure 1). No mediastinal involvement or distant metastasis where found. Preoperative tissue sample was obtained and the diagnosis of adenocarcinoma was established. The patient was offered a uniportal VATS right upper lobectomy and radical lymph node dissection (Figure 2). The pathology report confirmed the initial diagnosis and classified the disease as pT2aNoMo.
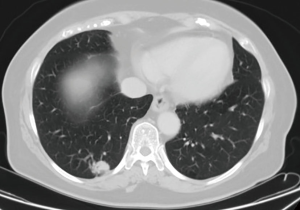
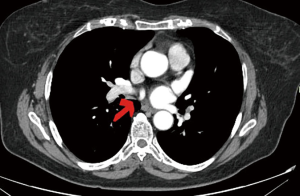
Case 2
A 71 years old female, non-smoker, who was diagnosed with a 1.3 cm, PET CT positive solitary pulmonary nodule at the right lower lobe, during her follow up for colon cancer for which she was treated with surgery and adjuvant chemotherapy. Because of her history, prior to the lobectomy, the lesion was removed via wedge resection and sent for frozen section to rule out the possibility of metastasis. The patient was then offered a uniportal VATS right lower lobectomy and radical lymph node dissection (Figure 3). The pathology report established the diagnosis of adenocarcinoma (pT1aNoMo). Intraoperatively an anomalous vein was noted, draining a subsegment of S6 directly into the left atrium (Figures 4,5).
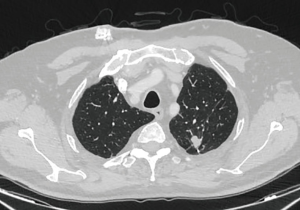
Case 3
A 66 years old male, past smoker, who was diagnosed with a 1.2 cm solitary pulmonary nodule at the left upper lobe (Figure 6). The patient had a history of resected colon cancer and had been submitted to wedge resection of a metastatic pulmonary nodule from the left upper lobe 18 months earlier. The new nodule seemed close enough to the stapler line, so a local relapse of the initial nodule was suspected. A wedge resection was performed. The pathology report confirmed the clinical scenario. The case was demanding as it was a redo and thus it served as a tutorial of how to manage complete and rigid adhesions via a minimally invasive manner. The author feels that an open approach would be more traumatic. The lung was totally adhered to the chest wall. The upper lobe was almost completely mobilized to locate and excise the lesion.
In all three cases the access was through the 5th intercostal space between the anterior and mid axillary line. Local anesthetic was infused at the intercostal space of the incision as well as at the intercostal spaces above and below it following the completion of the procedure.
Conclusions
The minimally invasive techniques are gradually emerging as the techniques of choice for the surgical treatment of lung cancer and are preferred over the open approach where experience is available (9). Amongst them the uniportal or single port technique is spreading rapidly. Its favorable geometric characteristics and imitation of the “eye over hands” sense of vision, along with a well-organized “training academy” running at the Shanghai Pulmonary Hospital are the main reasons. Surgeons operating via an anterolateral thoracotomy may familiarize easier with the technique. Surgical teams or individuals who are eager to adopt the technique should seek proctorship to ensure their success of their training. The tutoring of an expert cannot be replaced by surgical videos found at the social media, although the latter are indeed very helpful. The paradigm of the exponential spread of the single port VATS, offers a road map for how to massively train surgeons on a new technique removing financial and geographical barriers.
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Shah RD, D'Amico TA. Modern impact of video assisted thoracic surgery. J Thorac Dis 2014;6:S631-6. [PubMed]
- Rocco G, Khalil M, Jutley R. Uniportal video-assisted thoracoscopic surgery wedge lung biopsy in the diagnosis of interstitial lung diseases. J Thorac Cardiovasc Surg 2005;129:947-8. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Terzi A, et al. Geometric and ergonomic characteristics of the uniportal video-assisted thoracoscopic surgery (VATS) approach. Ann Cardiothorac Surg 2016;5:118-22. [Crossref] [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Soultanis CM, Gonzalez Rivas D, Konstantinidis K, et al. Uniportal right upper lobectomy and radical lymph node dissection. Asvide 2017;4:137. Available online: http://www.asvide.com/articles/1445
- Soultanis CM, Gonzalez Rivas D, Konstantinidis K, et al. Uniportal right lower lobectomy and radical lymph node dissection. Asvide 2017;4:138. Available online: http://www.asvide.com/articles/1446
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-313S.
Cite this article as: Soultanis CM, Rivas DG, Konstantinidis K, Siafakas K. The Athens uniportal video-assisted thoracic surgery masterclass—an ambitious kickstarter. J Vis Surg 2017;3:50.