Teaching uniportal video-assisted thoracic surgery in Rome
This article describes the tailored approach adopted at the “A. Gemelli” University Hospital in Rome in starting the uniportal video-assisted thoracic surgery (VATS) program. The training process in our experience has been made of two phases: the first one has been the attendance of special courses, like the International uniportal VATS Couse-Live Surgery and Wet-lab in Berlin (directed by Dr. D. Gonzalez-Rivas and Dr. M. Ismail) and the combined multilevel course at La Coruna (directed by Dr. D. Gonzalez-Rivas) and the second, the on-site surgical training (Proctorship) offered by Dr. Gonzalez-Rivas in our hospital.
Patient selection and workup
As result of the attendance of these advanced uniportal VATS courses, the uniportal VATS program of the “A. Gemelli” University Hospital-Catholic University of Sacred Heart of Rome was started, in May 2016.
After 20 uniportal VATS major lung resections, on the basis of the big enthusiasm generated among the thoracic staff, and looking forward to improve the technique, Dr. D. Gonzalez-Rivas was invited to make a personal proctorship at “A. Gemelli Hospital”.
Therefore, from 12 to 13 October 2016, Dr. Diego Gonzalez-Rivas spent 2 days with us, teaching his precious tricks as a special guest, in our operatory theatre.
During the 2-day surgical course Dr. Gonzalez Rivas worked alternatively as surgeon or assistant, teaching his precious tips and tricks at any passage (Figures 1-3). Four pulmonary lobectomies [1 upper right lobectomy, 1 middle lobe lobectomy (Figures 4,5), 1 upper right lobectomy en block with chest wall resection and 1 left upper lobectomy (Figures 6)] were performed.




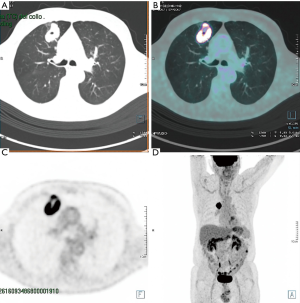
All cases, selected and discussed together with Dr. Gonzalez-Rivas before operation, were NSCLC in clinical stage I, except for the patient with chest wall invasion (Stage IIB-T3N0). All patients underwent complete preoperative evaluation including chest computed tomographic scan, PET scan and pulmonary function test. A 30-degree 10-mm video thoracoscope and high-definition imaging system were used together with dedicated thoracoscopic instrumentation by Scanlan (Scanlan International, Inc.) and Grena (Grena Ltd.). Medtronic provided the LigaSure™ Maryland and articulated endostapler (Endo Gia™ with Tri-staple™ Technology reloads).
Technique
All surgical procedures were performed under general anesthesia with double-lumen endotracheal tube placement for one-lung ventilation. The patients were placed in a lateral decubitus position. During operations, surgeon and assistant stood at the abdominal side of the patient, looking at the same monitor. The surgical incision (3.5−4.0 cm in length) was created in the fourth or fifth intercostal space at the anterior axillary line. A wound protector was routinely used, and no distraction device was employed to separate the ribs. The specimen was retrieved by a plastic bag through the incision wound. Conventionally, systematic mediastinal lymph node dissection was performed after lobectomy. All patients received intercostal nerve blockade with Ropivacaine and a 28 Fr chest tube was inserted at the end of the procedure. Patients were extubated immediately after the operation in the operating room. Postoperative outcome was uneventful. All patients were discharged in 3rd postoperative day.
Results
Since the introduction of uniportal VATS in our department in May 2016, we have performed more than 90 procedures; following the Dr. Gonzalez Rivas’s visit, uniportal VATS has replaced the open standard technique and triportal VATS in several procedures, up to major anatomic lung resections.
Uniportal VATS is actually reaching the role of preferred approach, whenever possible, for lung surgery at the Division of General Thoracic Surgery, “A. Gemelli” University Hospital, Catholic University of Sacred Heart of Rome.
Discussion
Minimally invasive surgery has been used in the past especially for diagnosis, palliative care or minor resections until the end of the 90s, when the first video assisted lobectomies were described (3). Many surgeons all over the world exposed their experience using VATS for minor and in particular major lung resections (4-6), starting the evolution of the technique, changing the geometry (7), the port number and the instruments to achieve visualization and an operating handling as comfortable as possible.
Finally, in 2012, Dr. Gonzalez-Rivas showed his good results using a uniportal VATS technique (7), reporting the feasibility of this approach for anatomic, major lung resections and, finally, complex procedures like double sleeve resections. The VATS evolution in our Institute matched the worldwide trend. Uniportal VATS shows many technical advantages when compared with open or triportal VATS approach: first of all, during uniportal VATS the axes of thoracoscopic view and instrumentations are parallel; this simulates the direct vision under open thoracotomy maneuver, and the eye-to-hand inconsistency would be the lowest among the other VATS approaches.
Moreover, uniportal VATS has the advantage of a common side and point of view between surgeon and assistant, making the assistant movements jointly connected with the operator perspective and reducing the number of aimless movements.
Despite these advantages, although surgeons are interested in adopting uniportal VATS, sometimes they may find difficulties both in the visualization and dissection of structures, as well as in the identification of the correct angles for instrumentation and endostapler deployment.
The most challenging aspect, in fact, moving from open surgery or triportal VATS to uniportal VATS is learning the fundamentals about the instruments dispositions through the wound retractor and the stapler angle.
Currently, realistic training opportunities involving multilevel courses, video libraries, hands-on conferences, and wet-lab experience are helping in uniportal VATS dissemination, and the combined course at La Coruna (8) is the best example of the highest level of training.
Following the attendance of the multilevel course, however, when a surgeon has learned fundamentals and started to perform uniportal VATS, it becomes of the foremost importance to be guided by skilled surgeons in creating the correct traction and use the appropriate instruments for every different passage during “real surgery” on the human being.
Moreover, during proctorship, the support personnel (OR nurse, anesthesiologist) are included in the training process; in order to master all the new approaches or techniques, training of the assistants, involvement of the multi-disciplinary team, introduction of appropriate complementary technology become of the foremost importance.
The presence of a proctor to guide or even personally undertake a particularly challenging stage enables the case to progress safely to the point when experience can be gained on the final stages. If a case fails at an earlier stage, this experience in the later stages is lost and a greater number of cases are required for competency in the later stages to be reached. On the other hand, Kwon et al. (9) reported that proctorship program has provided efficiency and rapid progression of learning curve among surgeons and proctorship training has been implicated on some curriculum to provide excellent progression during the learning curve while ensuring patient safety (10). It is therefore likely that for surgeon with significant pre-existing experience and knowledge, the proctoring visit act to consolidate learning and facilitate the transition from knowledge to practice. Although the increasing application of the uniportal VATS has brought about new challenges both for the surgeon and for the industry that provides us the technology to push the boundaries of surgery, it has also created unique opportunities for collaboration.
Acknowledgements
We want to thank Dr. D. Gonzalez-Rivas for his precious support in uniportal VATS program at the “A. Gemelli” University hospital. We also want to thank Medtronic for supporting the program financially.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Meacci E, Nachira D, Congedo MT, et al. Uniportal video-assisted thoracic surgery (VATS) upper right lobectomy with severe pleural adhesions. Asvide 2017;4:132. Available online: http://www.asvide.com/articles/1440
- Meacci E, Nachira D, Congedo MT, et al. Advanced instrumentation in lymphadenectomy. Asvide 2017;4:133. Available online: http://www.asvide.com/articles/1441
- Walker WS. Video-assisted thoracic surgery (VATS) lobectomy: the Edinburgh experience. Semin Thorac Cardiovasc Surg 1998;10:291-9. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Sihoe AD, Tan HY. Complete Video Assisted Thoracic Surgery Major Lung Resection for Lung Cancer: the impact of Tuberculosis and Post-inflammatory Adhesions on outcomes. Respirology 2011;16:138. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- Eckland K, Gonzalez-Rivas D. Teaching uniportal VATS in Coruña. J Vis Surg 2016;2:42. [Crossref]
- Kwon EO, Bautista TC, Blumberg JM, et al. Rapid implementation of a robot-assisted prostatectomy program in a large health maintenance organization setting. J Endourol 2010;24:461-5. [Crossref] [PubMed]
- Santok GD, Raheem AA, Kim LH, et al. Proctorship and mentoring: Its backbone and application in robotic surgery. Investig Clin Urol 2016;57:S114-S120. [Crossref] [PubMed]
Cite this article as: Meacci E, Nachira D, Congedo MT, Margaritora S. Teaching uniportal video-assisted thoracic surgery in Rome. J Vis Surg 2017;3:49.