Totally laparoscopic total gastrectomy for locally advanced middle-upper-third gastric cancer
Introduction
There are great advantages in totally laparoscopic gastrectomy in exposure, pulling, surgical field, and less invasive effects over laparoscopy-assisted surgery (1-6). Hence, this method has been attracting more and more attention from laparoscopic experts. Totally laparoscopic total gastrectomy (TLTG) for locally advanced middle-upper-third gastric cancer is becoming increasingly popular. However, there are some difficulties preventing the development. The main difficulties of TLTG for locally advanced middle-upper-third gastric cancer lay in the laparoscopic spleen-preserving splenic hilar lymphadenectomy and the intracorporeal digestive tract reconstruction (7-10). Hence, we summed up a set of unique experience through clinical practice to simplify operation procedures.
Patient selection and workup
The TLTG with Huang’s three-step maneuver in laparoscopic spleen-preserving splenic hilar lymphadenectomy and a later-cut overlap Roux-en-Y anastomosis in the intracorporeal digestive tract reconstruction is indicated for patients with locally advanced middle-upper-third gastric cancer. The invasion of esophagus should be less than three center meters. And the patients with T4b tumors, enlargement or integration of lymph nodes (LNs) around the stomach or intraoperative evidence of peritoneum and pelvic implantation metastasis or distant metastasis are not suitable for surgery. Preoperative workups include hematological examinations, electrocardiogram, chest radiography, computed tomography scan, pulmonary function test, abdominal ultrasonography, gastrointestinal radiography film with diatrizoate meglumine, endoscopic examination and endoscopic biopsy specimens to evaluate the situation of patient comprehensively.
Pre-operative preparation
After routine preoperative preparation, the endotracheal intubation and general anesthesia are performed. The patient is in the supine position with head elevated 10–20° and the legs apart. During the dissection of the splenic hilar LNs, the upper body of patient is elevated approximately 10–20°, and the left-side body is tilted up 20 to 30 degrees. Generally, we use 5-port to set trocars. The establishment of pneumoperitoneum uses 12–14 mmHg carbon dioxide. Generally, the surgeon stands on the left side of patient, the assistant stands on the right side of patient, and the camera assistant stands between the legs of patient. While when dissect the splenic hilar LNs, the assistant and camera assistant both stand on the right side of patient, and the surgeon is placed between the patient’s legs (Figure 1).

Equipment preference card
Routine laparoscopic devices include the camera and display systems, the image and video storage equipment, the pneumoperitoneum machine, the suction and irrigation equipment, five 5–12-mm trocars, an aspirator, noninvasive grasping forceps, Maryland forceps, intestinal forceps, a needle holder, scissors, a titanium clip applier, an absorbable clip applier, vascular clamps, and small gauzes. Special devices include ultracision, bi-active coagulation set, LigaSureTM vessel sealing system, and endoscopic linear staplers.
Procedure
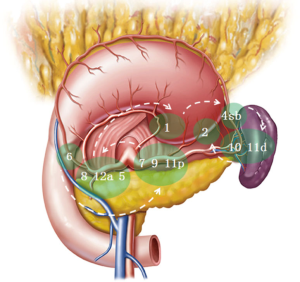
Firstly, the laparoscopic exploration should be performed to confirm the tumor site and exclude T4b gastric cancer or metastasis to other organ, such as the abdominal cavity, the liver or pelvic cavity. LNs dissection is performed according to the guidelines of Japanese Gastric Cancer Association. The sequence of lymph node dissection in total gastrectomy is from No. 6 LNs to No. 7, 9, 11p LNs, then to No. 8a, 12a, 5 LNs, next to No. 1 LNs, and to No. 4sb LNs, then to No. 10, 11d LNs, and last to No. 2 LNs (Figure 2).
We performed Huang’s three-step maneuver during laparoscopic spleen-preserving splenic hilar lymphadenectomy. This new maneuver simplifies the complicated procedure and improves the efficiency of laparoscopic spleen-preserving splenic hilar lymphadenectomy, making it easier to grasp and popularize. The Huang’s three-step maneuver divided the complicated procedure of laparoscopic spleen-preserving splenic hilar lymphadenectomy into three steps, including the dissection of the LNs in the inferior pole region of the spleen (1st step), the region of the splenic artery trunk (2nd step), and the superior pole region of the spleen (3rd step).
First step
The assistant pulls the gastrosplenic ligament, while the surgeon presses the pancreas’ tail. The greater omentum is separated along the superior edge of transverse mesocolon until to splenic flexure of the colon. Then peel the anterior pancreatic fascia from the pancreas to the superior edge of the pancreatic tail. Next, the peeled the anterior pancreatic fascia and the anterior lobe of the transverse mesocolon are completely placed to the cephalad, to reveal the lower pole vessels or lower lobar vessels of the spleen. Then dissect these lymphatic tissues on the surface of the vessels. During the dissection, the left gastroepiploic vessels can then be exposed and denuded completely. Next, transect the left gastroepiploic vessels at their roots to accomplish the resection of No. 4sb LNs. Then as the lower lobar vessels of the spleen are gradually exposed, divide 1–2 branches of the short gastric vessels at their roots when encounter them.
Second step
The assistant pulls the greater curvature of the fundus toward the upper right, while the surgeon presses the pancreas’ body to expose the splenic artery area in the retropancreatic space. Then the fatty lymphatic tissue is dissected on the surface of splenic artery trunk, from middle to the splenic lobar arteries’ crotch along the latent anatomic spaces. During the dissection, the surgeon will denude and divide the posterior gastric artery deriving from the splenic artery. After the fatty lymphatic tissue on the splenic vessels is completely dissected, the dissection of No. 11d LNs is accomplished.
Third step
The assistant pulls the greater curvature of the fundus toward the lower right, while the surgeon presses the splenic hilum’s vessels to reveal the superior pole region of spleen. Then in the splenic superior lobar area, denude the splenic vessels’ branches in the gastrosplenic ligament. One to three branches of the short gastric vessels arise from the splenic vessels’ terminal branches will always be encountered during this time; dissect the fatty lymphatic tissue around the vessels and divide the vessels at their roots. The last short gastric vessel is often very short and easy to damage in the superior pole region of spleen, which often causes bleeding. The splenic hilar lymphadenectomy is accomplished after completely dissecting the fatty lymphatic tissue of the splenic hilar.
After dissecting the LNs under laparoscopic we start to perform digestive tract reconstruction in the abdominal cavity.
Firstly, we mobilize the esophagus and the duodenum. Then transect them using the endoscopic linear staplers in predetermined positions respectively. Secondly, we made small incisions on the resection margin’s left side of the esophagus and the antimesenteric border of the jejunum where about 20 cm away from Treitz ligament. Thirdly, we insert the endoscopic linear stapler from the main operating hole. After inserting one limb of the stapler in each incision, the stapler’s forks are closed and fired to carry out the side-to-side esophagojejunostomy. Confirm that there is no bleeding or no injuring via the common stab incision; we manual suture the common stab. Fourthly, after baring the mesenteric border about 1 cm in the jejunum wall where about 7 cm away from esophagojejunostomy, transect the jejunum here. The essence of a later-cut overlap Roux-en-Y anastomosis is that the small intestine is cut off after the esophagojejunostomy is completed, so that we can grasp the small intestine more easily and determine the direction of anastomosis more conveniently. Next, we make the second anastomosis. After made the small incision on the antimesenteric border of the proximal jejunum’s margin and distal jejunum where about 40–45 cm away from esophagojejunostomy, inserting one limb of the stapler in each incision, closed and fired the forks of the stapler to achieve the side-to-side jejunojejunostomy. Confirm that there is no bleeding or no injuring to the jejunal mucosa via the common stab incision. Then suture the common stab incision under laparoscopy. Finally, we remove the specimen by the 3.5 cm incision of median incision on upper abdomen. In this way, the isoperistaltic later-cut Roux-en-Y anastomosis in TLTG is completed (Figure 3).
Role of team members
The surgeon is responsible for the operation. The assistant is responsible for the exposure and assistance. And the camera assistant is responsible for providing high quality images.
Post-operative management
On postoperative day (POD) 2 remove the Foley catheter. On POD 3–4 the gastric tube is removed after the first flatus, and diet advanced to a nasal feeding liquid diet (100–200 cc/2 h). On POD 5 oral liquid diet is allowed. On POD 7 the patient is advance to a semifluid diet. On POD 8 the abdominal drainages are removed. On POD 9 the nasogastric tube is removed and the patient was discharged home.
The evaluation of safety and feasibility
One patient experienced later anastomotic leakage and was successfully treated by conservative in 16 consecutive patients. No patient experienced any operation-related complications. At a median follow-up of 15 months, no patients had died or experienced recurrent or metastatic disease. Preliminary results showed that, TLTG with Huang’s three-step maneuver in laparoscopic spleen-preserving splenic hilar lymphadenectomy and a later-cut overlap Roux-en-Y anastomosis in the intracorporeal digestive tract reconstruction for locally advanced middle-upper-third gastric cancer was technically safe and feasible, with acceptable short-term outcomes.
Tips, tricks and pitfalls
- Due to the narrow and deep space in the spleen hilum, complexity of the splenic hilar vessels, as well as the bleeding-prone splenic parenchyma and the difficulty to manage splenic or vascular bleeding at the splenic hilum, laparoscopic spleen-preserving splenic hilar lymphadenectomy in situ needs high requirement of surgical skills. This procedure is recommended to be carried out only by surgeons with rich experience in open operations and skilled laparoscopic surgical techniques;
- The “chopsticks effect” phenomenon is often occurred, because the area in the left upper abdomen is narrow, and the surgeon’s and assistant’s instruments point together with a small angle between them into the area. At this time, the camera assistant should avoid this situation by adjusting the optical fiber and lens to avoid this situation;
- The surgeon, assistant, and camera should cooperate closely to successfully perform the Huang’s three-step maneuver;
- The transection line was vertical to the long axis of the esophagus and jejunum;
- We first insert one limb of the 60 mm endoscopic linear stapler into the jejunum incision because of the greater mobility of the jejunum, then the other limb is placed on the esophagus;
- Before leaving we checked the anastomotic tension and quality, and close the mesenteric hiatal by laparoscopic continuous or interrupted suture.
Acknowledgements
Funding: This study supported by Scientific and technological innovation joint capital projects of Fujian Province (2016Y9031).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee (No. 2016KY049) and written informed consent was obtained from all patients.
References
- Song KY, Park CH, Kang HC, et al. Is totally laparoscopic gastrectomy less invasive than laparoscopy-assisted gastrectomy?: prospective, multicenter study. J Gastrointest Surg 2008;12:1015-21. [Crossref] [PubMed]
- Ikeda O, Sakaguchi Y, Aoki Y, et al. Advantages of totally laparoscopic distal gastrectomy over laparoscopically assisted distal gastrectomy for gastric cancer. Surg Endosc 2009;23:2374-9. [Crossref] [PubMed]
- Kinoshita T, Shibasaki H, Oshiro T, et al. Comparison of laparoscopy-assisted and total laparoscopic Billroth-I gastrectomy for gastric cancer: a report of short-term outcomes. Surg Endosc 2011;25:1395-401. [Crossref] [PubMed]
- Kanaji S, Harada H, Nakayama S, et al. Surgical outcomes in the newly introduced phase of intracorporeal anastomosis following laparoscopic distal gastrectomy is safe and feasible compared with established procedures of extracorporeal anastomosis. Surg Endosc 2014;28:1250-5. [Crossref] [PubMed]
- Kim HS, Kim MG, Kim BS, et al. Comparison of totally laparoscopic total gastrectomy and laparoscopic-assisted total gastrectomy methods for the surgical treatment of early gastric cancer near the gastroesophageal junction. J Laparoendosc Adv Surg Tech A 2013;23:204-10. [Crossref] [PubMed]
- Okabe H, Obama K, Tsunoda S, et al. Advantage of completely laparoscopic gastrectomy with linear stapled reconstruction: a long-term follow-up study. Ann Surg 2014;259:109-16. [Crossref] [PubMed]
- Hyung WJ, Lim JS, Song J, et al. Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg 2008;207:e6-11. [Crossref] [PubMed]
- Okabe H, Obama K, Kan T, et al. Medial approach for laparoscopic total gastrectomy with splenic lymph node dissection. J Am Coll Surg 2010;211:e1-6. [Crossref] [PubMed]
- Tsunoda S, Okabe H, Obama K, et al. Short-term outcomes of totally laparoscopic total gastrectomy: experience with the first consecutive 112 cases. World J Surg 2014;38:2662-7. [Crossref] [PubMed]
- Kim HS, Kim MG, Kim BS, et al. Totally laparoscopic total gastrectomy using endoscopic linear stapler: early experiences at one institute. J Laparoendosc Adv Surg Tech A. 2012;22:889-97. [Crossref] [PubMed]
- Lin M, Huang CM, Zheng CH, et al. Totally laparoscopic total gastrectomy (TLTG) with Huang’s three-step maneuver in laparoscopic spleen-preserving splenic hilar lymphadenectomy and a later-cut overlap Roux-en-Y anastomosis. Asvide 2017;4:130. Available online: http://www.asvide.com/articles/1438
Cite this article as: Lin M, Huang CM, Zheng CH, Li P, Xie JW, Chen QY, Huang ZN. Totally laparoscopic total gastrectomy for locally advanced middle-upper-third gastric cancer. J Vis Surg 2017;3:46.