New stapling devices in robotic surgery
Introduction
Minimally invasive anatomic pulmonary resection (lobectomy and segmentectomy) has become a standard of cure for the treatment of early stage lung cancer and robotic resection is gaining popularity and acceptance among different minimally invasive techniques in the thoracic community. These less-invasive procedures are technically feasible and safe procedures with good surgical and oncological outcomes as shown by international experiences (1-4).
A new robot device, da Vinci Xi System has been recently released by Intuitive Surgical (Inc., Sunnyvale, CA, USA). One of the most important technical, practical, and useful innovation which accompanied this new robotic system is the use of robotic stapler (EndoWrist Stapler) directly controlled by the surgeon. To date, only one recent report has reported the use of this new device (5). The goal of our study was to illustrate our recent experience in the use of EndoWrist Stapler during robotic anatomic surgery for lung cancer reporting our operative technique and early surgical results in a large case series.
Patient selection and workup
We prospectively evaluated the use of robotic stapler in a cohort of patients with early lung cancer who were scheduled to have a robotic anatomic pulmonary resection (lobectomy or segmentectomy) between February and November 2016.
Patients with suspected or proven clinical stage I or II lung cancer were recruited to undergo robotic lobectomy provided they satisfied the following inclusion criteria: lesion less than 4 cm, normal respiratory function (including forced expiratory volume in 1 second greater than 65% of predicted), nor prior thoracic surgery, no neoadjuvant treatment, no need for extended or sleeve resection. All patients underwent complete preoperative staging including whole body computed tomography, positron emission tomography, tissue diagnosis by bronchoscopy (brushing or biopsy) or through transthoracic needle biopsy. Endobronchial ultrasound was performed both for diagnosis of the tumor or in case in which visual assessment of positron emission tomography scans suggested mediastinal adenopathy. All patients received also standard haematology and blood chemistry, cardiologic and pneumologic examination. In general, segmentectomy was planned for patients with marginal pulmonary reserve or those with lesion 2 cm or less.
Technique
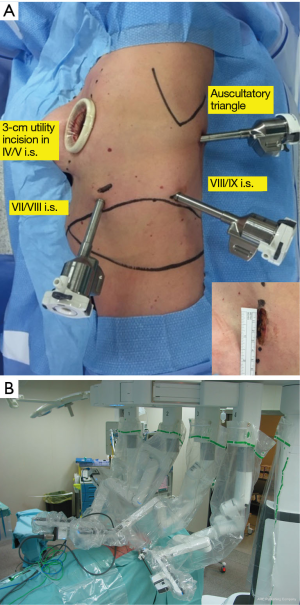
All procedures were performed under general anaesthesia with a double-lumen endotracheal tube. Patient and personnel were positioned as previous reported (3). Briefly, after a lateral decubitus, a 3-cm utility incision was made at the 4th or 5th intercostal space, anteriorly. Through this incision the 8-mm 30° tridimensional robotic endoscope was inserted into the chest to explore the pleura and to help to made under direct vision the three other ports: 8-mm incision for the camera port in 7th–8th intercostal space in the midaxillary line; two other ports were placed at the 8th–9th intercostal space in the posterior axillary line and at the auscultatory triangle, respectively (Figure 1A). With the new robotic system, it is not import to respect a particular distance between two ports, because the new da Vinci Xi may work also with a minimum distance of 4 cm between them. Portal placement did not change with segmentectomy or side, except for left side operations where camera port was placed more laterally to keep the heart out of way. A 12-mm port was used for EndoWrist stapler: for inferior lobectomy and segmentectomy it was placed alternatively at the utility thoracotomy or posterior axillary line; for the upper lobectomy, it was placed at the posterior axillary line. The manufacturer makes plastic reducers that fit inside the 12-mm port and house 8-mm instruments during the operation. The reducers are easily removed for insertion of the stapler. In every case the surgical cart was docked from the left side of the patient (Figure 1B) either for right or left thoracic procedures taking advantage of the technical innovation of this new robotic system to displace correctly the four arms despite its side position.
Below, we describe the various types of anatomic pulmonary resections reporting the different steps, the port used in each procedure, and the type of cartridges used:
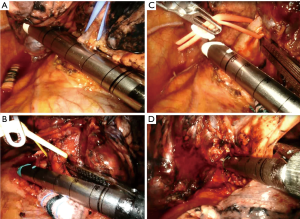
Left upper lobectomy: the first step was dissection of pulmonary vein and its suture/resection introducing robotic vascular stapler (45 mm, white cartridge) through the posterior axillary port (Figure 2A). The first pulmonary artery branch was then dissected and sutured/resected with the same cartridge and through the same port access (Figure 2B). Other arterial branches for the upper lobe were eventually identified and legated by Hem-o-lok (Weck Surgical Instruments, Teleflex Medical, Durham, North Carolina, USA). Peribronchial nodes were removed. Bronchus for upper lobe was dissected, encircled and sutured/resected by a 45 mm green cartridge (Figure 2C). Fissure was then divided by 45 mm green or blue cartridges either entering through posterior axillary port (Figure 2D). A robotic left upper lobectomy with the use of EndoWrist staplers 40 mm is reported (Figure 3).
Right upper lobectomy: the technique was the same before described except for the timing of bronchial resection which was performed after the first arterial brunch resection. Fissure was then divided by 45 mm green or blue cartridges either entering through utility thoracotomy or posterior axillary port.
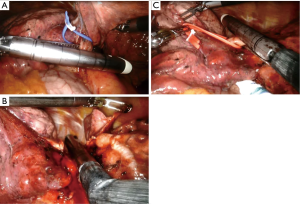
Inferior right/left lobectomy: pulmonary vein was transected introducing the robotic stapler through utility thoracotomy (Figure 4A); after the completion of the anterior portion of the fissure performed by electrocautery or 45 mm green robotic stapler, arterial branches for inferior lobe, lobar bronchus, and fissure were transected by introducing robotic stapler (45 mm, white cartridge and green, respectively) through utility thoracotomy or posterior axillary port (Figure 4B,C).
Middle lobectomy: anterior fissure was transected by 45 mm green cartridge introduced by dorsal port (Figure 5A). Vein and bronchus were transected by introducing robotic stapler (45 mm, white cartridge and green, respectively) through posterior axillary port (Figure 5B,C), while arterial branches were ligated by Hem-o-lok or robotic stapler introduced by the dorsal port (Figure 5D). Fissure was completed by 45 mm green cartridge introduced by utility thoracotomy or dorsal port.

Lingulectomy: lingular segmental vein was dissected and sutured/resected by a robotic vascular stapler (45 mm, white cartridge) through the posterior axillary port; the segmental bronchus was isolated and stapled through posterior axillary port by a 45 mm green cartridge; after the fissure dissection, the lingular arterial branch was isolated and stapled through utility thoracotomy or posterior axillary port with the vascular robotic stapler. Transection of the parenchyma was performed as the last step, with the robotic stapler introduced through anterior utility thoracotomy (usually, 45 green cartridges).
Right lower lobe/Left lower lobe superior segmentectomy: superior segmental vein was dissected and sutured/resected through the posterior axillary port; the segmental bronchus was isolated and stapled through posterior axillary port; the segmental arterial branch was isolated and stapled through utility thoracotomy or posterior axillary port. Transection of the parenchyma was performed as the last step, with the robotic stapler introduced through anterior utility thoracotomy (45 green cartridges).
From September 2006, 30 mm robotic EndoWrist Stapler with 30 mm reloads with curved and straight tip were available at our Institution and routinely used for vascular and bronchial robotic resection. EndoWrist Stapler 45 mm is actually used in our practice to complete the fissure.
Experience
During the period February and November 2016, a total of 92 anatomic pulmonary robotic resections have been performed by both da Vinci Xi (n=60) and da Vinci Si (n=32) System. Of those performed by da Vinci Xi, 45 patients underwent robot-assisted lung anatomic resection with the use of robotic stapler. There were 21 men, and 24 women. Mean age was 67.4 years (range, 41–83 years). Mean docking time was 4.1 minutes (range, 3–7 minutes), while mean operative time was 175 minutes (range, 90–240 minutes). We performed 4 segmentectomies, 26 upper lobectomies (12 right, 14 left), 13 lower lobectomies (7 right and 6 left), and 2 median lobectomies. No conversion to thoracotomy was required. Median chest tube duration was 3 days (range, 2–21 days). Median postoperative length of stay was 5 days (range, 3–21 days). Postoperative morbidity included three cases of prolonged air leaks (all with history of pulmonary emphysema and BPCO), three cases of atrial fibrillation, and two cases of pneumonia. Histology included 35 adenocarcinomas, 5 squamous cell carcinomas, 3 carcinoids, 1 adenosquamous carcinoma, and 1lymphoma.
Comment
Intuitive Surgical, Inc., Sunnyvale, CA, USA, the pioneer in the robotic technology, released in early 2014 the new da Vinci Xi gaining the approval by the US Food and Drug administration for its use. This new device, da Vinci Xi, is an improvement of the previous ones: the docking is simpler and is designed to be user friendly, guided by a “port placement menu” and a laser. The scope has a digital end-mounted camera for improved vision and requires no draping and can be placed into any of the robotic arms and has autofocus. Because of the improved design for the arms, the ports can be placed relatively close together and still avoid collision.
The main innovation which accompanied the new robotic device (da Vinci Xi) has been the introduction of EndoWrist Stapler. In the previous robotic thoracic experiences (1-4), in all the cases, vessels, bronchus and incomplete fissures were sutured and sectioned by EndoGia stapler introduced by the assistant surgeon through one of the port after removal of a robotic arm. To date, only one recent report has reported the use of this new device outlining the early experience using the robotic stapler and providing techniques that have maximized efficiency and safety when using these staplers (5).
The first robotic stapler system has been a 45 mm EndoWrist Stapler. Only recently, a new EndoWrist Stapler 30 mm has become available. The EndoWrist Stapler, both 30 mm and 45 mm, is introduced into the operative field by the assistant surgeon as a simple robotic instrument through a 12 mm port. It is fully controlled by surgeon’s hands through the da Vinci Xi System and provides fully wristed articulation and SmartClamp feedback. This stapler has the greatest side-to-side articulation currently available, with a range of 108° total side-to-side. And unlike other staplers currently available, the EndoWrist Stapler articulates through a range of 54° total up-and-down. The fully wristed articulation enables precise positioning around vital structures. The EndoWrist Stapler Reloads include a microchip which automatically tells the da Vinci System what reload color is installed and will not allow the system to fire an incorrectly loaded or spent stapler reloads. Three different EndoWrist Stapler reloads are currently available (white, blue and green) which correspond to the same closed-staple heights of the equivalent reload colors available in the current market.
In our experience, because the stapler’s end effector is considerably longer than other robotic instruments, it is advantageous to have the stapling ports as low as possible (close the diaphragm) and to insert the instrument deeply in the chest and moving it with great attention; this allow the greatest degree of maneuverability in the chest avoiding lung and vascular damages.
Smart Clamp feedback helps in achieving a full clamp by detecting if stapler jaws are adequately closed on target tissue for selected reload color prior to firing; it seems more useful for parenchymal resection then vessels/bronchus. When it fails to achieve 100% of clamping, we re-open the jaws and re-close them so as achieve an adequate closure on target tissue. The EndoWrist Stapler Reloads for the da Vinci Xi System include a microchip that will not let the system fire an incorrectly loaded or spent stapler reloads.
In addition to the difficulties in articulating the EndoWrist Stapler deriving from length of stapler’s tip (this is true for the 45 mm stapler, other drawbacks of robotic stapler are: (I) rotational limitation may occur when arm is flexed at extreme and this situation causes a dangerous jerking movement; (II) time consuming during reload replacing (if residual staples are not well removed after firing), in calibrating and firing each load, in correctly positioning a protective sheath (a small fold may lock the device).
Comparing EndoWrist stapler versus endostapler, we can say that robotic stapler (I) is a useful device; (II) it has simplified pulmonary resection by direct control by the surgeon avoiding assistant’s handling at bedside; and this (III) provides surgeon to perform anatomic pulmonary resections in safer conditions.
The issue of robotic and stapler cost, availability, training, and lack of haptic feedback must be offset by the improved efficiency of operation, safety of the anatomic resection, and by the direct control on the suture of anatomic structures.
In our experience, we see potential for improvement in each of these areas above all by the use of the EndoWrist Stapler 30 mm. This new robotic instrument simplifies the suture and resection of vascular and bronchial structures rendering the robotic anatomic resection safer, simpler, and rapid.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Park BJ, Flores RM, Rusch VW. Robotic assistance for video-assisted thoracic surgical lobectomy: technique and initial results. J Thorac Cardiovasc Surg 2006;131:54-9. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Starting a robotic program in general thoracic surgery: why, how, and lessons learned. Ann Thorac Surg 2011;91:1729-36; discussion 1736-7.
- Veronesi G, Galetta D, Maisonneuve P, et al. Four-arm robotic lobectomy for the treatment of early-stage lung cancer. J Thorac Cardiovasc Surg 2010;140:19-25. [Crossref] [PubMed]
- Melfi FM, Fanucchi O, Davini F, et al. Robotic lobectomy for lung cancer: evolution in technique and technology. Eur J Cardiothorac Surg. 2014;46:626-30; discussion 630-1. [Crossref] [PubMed]
- Pearlstein DP. Robotic Lobectomy Utilizing the Robotic Stapler. Ann Thorac Surg 2016;102:e591-e593. [Crossref] [PubMed]
- Galetta D, Casiraghi M, Pardolesi A, et al. A robotic left upper lobectomy with the use of EndoWrist staplers 45 mm. Asvide 2017;4:125. Available online: http://www.asvide.com/articles/1433
Cite this article as: Galetta D, Casiraghi M, Pardolesi A, Borri A, Spaggiari L. New stapling devices in robotic surgery. J Vis Surg 2017;3:45.


