Educational system of laparoscopic gastrectomy for trainee—how to teach, how to learn
Introduction
Laparoscopic gastrectomy (LG) are firstly reported by Kitano et al. in 1994 (1) and now widely spread to East Asian countries. Japan Society for Endoscopic Surgery (JSES) reported 34.0% of the gastrectomy for gastric cancer is performed under laparoscopy in Japan, in 2013. Laparoscopic distal gastrectomy (LDG) for early gastric cancer has been accepted as a standard procedure for experienced laparoscopic surgeons following the results of feasibility studies conducted in Japan and Korea (2,3). Although low complication rate was shown in these trials, the surgeons who performed surgery included in these studies were so-called “expert’’ surgeons because the criteria as for operator in these trials was restricted to surgeons with experiences of at least 30–80 laparoscopic gastrectomies. Feasibility of laparoscopic surgery performed by trainee is still debatable and only a few studies had been existed so far describing its educational system. It is reported that less than 50% of educational institution of LG in Japan and Korea adopt their own educational program for trainee (4). Here we report our own educational system for LG for trainee in our hospital.
Early period after introduction of LG in our institution
We introduced LG for gastric cancer in 2010, and recently our hospital became one of the high-volume centers regarding LG in Japan. Standardized procedure was introduced by an expert surgeon. Standardized surgical procedure and environment are described in “laparoscopic manuals’’ edited in our institution, which could be shared not only with surgeons but with surgical co-medicals, such as nurses or medical engineer, finally established a “laparoscopic team’’. As surgical procedures or used devices were improved and changed, these contents were reflected to our manual. The significance of team participation training system was reported previously by us (5).
Characteristics of our residency program
Around 300 cases of gastrectomy for gastric cancer are performed annually and currently 70–80% of the cases are operated laparoscopically. Trainee who wants to work in our division usually apply for our residency program at 5–8 post-graduation years after they have acquired the board certification from Japan Surgical Society. Our residency program consists of 3 years program as junior resident and 2 years program as senior resident. In the first 2 years of the junior residency program, actually they work at gastric surgery division only for 6 months, and for the rest period rotate in other surgical divisions (esophageal, hepato-biliary pancreatic and colorectal surgery), pathological division and medical oncological division to learn widely oncology and basic skills of gastroenterological surgery.
The last year of junior resident are specialized in the training program of gastric surgery division. Senior residency program are aiming to more deepen their knowledge and skills as gastric surgeons.
Three factors for mastering laparoscopic surgery
Learning, practice and experience are the three indispensable factors for mastering LG as shown in Table 1.
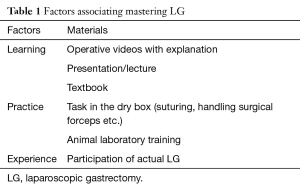
Full table
‘’Learning’’: learn the standardized procedure
Trainees learn the standardized reproducible procedure thorough the non-edited operative video performed by trainer repeatedly as well as textbook to learn ideal exposure of operative field. The typical exposure of operative field for supra pancreatic lymph node dissection are demonstrated in Figure 1.

“Practice’’: practice using the dry box
Trainee should practice laparoscopic suturing techniques or handling of surgical devices through the training using the dry box. Hand-eye coordination and peculiar movement of laparoscopic surgery could be acquired by effective creative tasks in the dry box before participating in actual surgery as shown in Figure 2.
“Experience’’: participate in actual laparoscopic surgery
In our division, junior resident participate in laparoscopic surgery basically as a scopist in their first year. After they experienced five to ten cases as a scopist and understood the standardized procedure, they can promote to an assistant of LDG or an operator of easier laparoscopic surgery, such as staging laparoscopy or laparoscopic gastrojejunostomy. At the same time, they can also experience open gastrectomy as well. Trainee performs their first LDG as an operator after ten to twenty experiences as assistant. At the third year of junior resident or the first year of senior resident, they can take the examination to obtain certification of endoscopic surgical skill qualification system of JSES (8). Training program of our residency system was summarized in Figure 3.

The principles for our surgical team to play each role in laparoscopic surgery
We have following common principles and concepts as described below.
The principles for scopist
Show the typical view
A 10 mm flexible scope is routinely used in our institution. The operator and the assistant have to make the standardized operative field, and the scopist have to show these reproducible operative fields. Discrepancy of the typical view shown by scopist could lead to misunderstanding of surgical anatomy, which may be associated with unexpected injury of other organs.
Avoid collision between scope and other surgical devices
Scopist should recognize intraabdominal positional relationship of each surgical device, and control scope position not to conflict with other devices. This principle must be recognized by operator and assistant as well, always considering provision of space for scope.
Show surgical devices not blindly
Any energy devices have possibility to give thermal injury to other organs, such as pancreas or major vessels due to blind activation and cavitation. Scopist should pay maximum attention to show the active blade of energy devices as possible to avoid blind procedures. For this, articulating function of the flexible scope is very useful.
The principles for assistant
Basic step of assistant begins with exposure of typical operative field in LDG for early gastric cancer. More advanced procedures, such as total gastrectomy with splenic hilar dissection for advanced gastric cancer, require more complicated exposure of surgical field, thus assistant should understand surgical anatomy and operative procedure very well. The principles for assistant which are decided in our institution to expose the good operative field are as follows.
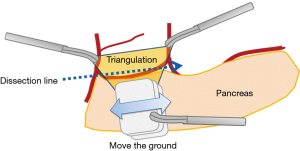
Triangulation and move the ground
Triangle formation to expose the operative field with proper tension can be made using two forceps handled by assistant and left hand forceps of operator (triangulation). In laparoscopic surgery, the axis of surgical device is fundamentally fixed by the trocar. Thus, operator and assistant should adjust the dissection line to the axis of surgical energy devices driven by operator’s right hand by moving organs (move the ground) as shown in Figures 4,5. Delicate organs, such as pancreas, should be handled gently using gauze grasped by assistant to prevent related complications, such as pancreatic leak or pancreatitis.
The principles for operator
Needless to say, basic skills, such as stable movement of forceps/energy devices, vessel ligation or hemostatic techniques, should be mastered. Moreover, advanced surgical knowledge regarding lymph node dissection (proper dissection layer, anatomical landmark) or reconstruction (intracorporeal stapling techniques) should be fully understood.
How to teach and how to learn the laparoscopic surgery efficiently?
Because of the complexity of the relevant anatomy, LG had been thought to be difficult to be learned or performed by young surgeons. Detailed standardization of the procedure not only for surgeons but also for co-medical staffs seems to play a pivotal role for it. Although in several situations in actual clinical surgery standardized procedure will not fit due to tumor progression or patient’s specific condition, such as obesity, fragility of tissue and adhesion. However, if the principle for surgical performance is decided and shared by surgical team, we can overcome tough situation. Trainer should make effort to teach these methods to trainee using understandable key words such as “triangulation”, “move the ground’’, “no conflict’’ repeatedly. Trainees should fully understand meanings of these words and practice task in the dry box with purposes, and discuss with trainer or other surgical team members.
In conclusion, we believe, combination of the three factors “learning’’, “practice’’ and “experience’’ are the key words for mastering LG. Trainer should transmit standardized reproducible procedures to trainee using understandable words repeatedly, and trainee should trace trainer’s manner repeatedly.
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kitano S, Iso Y, Moriyama M, et al. Laparoscopy-assisted Billroth I gastrectomy. Surgical laparoscopy & endoscopy 1994;4:146-8. [PubMed]
- Kim W, Kim HH, Han SU, et al. Decreased Morbidity of Laparoscopic Distal Gastrectomy Compared With Open Distal Gastrectomy for Stage I Gastric Cancer: Short-term Outcomes From a Multicenter Randomized Controlled Trial (KLASS-01). Ann Surg 2016;263:28-35. [Crossref] [PubMed]
- Katai H, Sasako M, Fukuda H, et al. Safety and feasibility of laparoscopy-assisted distal gastrectomy with suprapancreatic nodal dissection for clinical stage I gastric cancer: a multicenter phase II trial (JCOG 0703). Gastric Cancer 2010;13:238-44. [Crossref] [PubMed]
- Lee HJ, Shiraishi N, Kim HH, et al. Standard of practice on laparoscopic gastric cancer surgery in Korea and Japan: experts' survey. Asian J Endosc Surg 2012;5:5-11. [Crossref] [PubMed]
- Kinoshita T, Kanehira E, Matsuda M, et al. Effectiveness of a team participation training course for laparoscopy-assisted gastrectomy. Surg Endosc 2010;24:561-6. [Crossref] [PubMed]
- Kaito A, Kinoshita T. Typical educational video. Asvide 2017;4:026. Available online: http://www.asvide.com/articles/1332
- Kaito A, Kinoshita T. Suture training in dry box. Asvide 2017;4:027. Available online: http://www.asvide.com/articles/1333
- Tanigawa N, Lee SW, Kimura T, et al. The Endoscopic Surgical Skill Qualification System for gastric surgery in Japan. Asian J Endosc Surg 2011;4:112-5. [Crossref] [PubMed]
- Kaito A, Kinoshita T. The concept of “triangulation’’ and “move the ground’’ in dry box. Asvide 2017;4:028. Available online: http://www.asvide.com/articles/1334
Cite this article as: Kaito A, Kinoshita T. Educational system of laparoscopic gastrectomy for trainee—how to teach, how to learn. J Vis Surg 2017;3:16.


