The Zakopane Pulmonary Hospital experience on subxiphoid thymectomy
Introduction
We started to use the subxiphoid incision for thymectomy in 2000. By that time we had been using the extended transternal approach similar to that described by Bulkley et al. (1). We proved that this extensive technique resulted in the improved complete-remission rate in comparison to our previous basic thymectomy approach consisting of the removal of the sole thymus gland, without the surrounding adipose tissue performed through the upper sternal split (2). Considering the expectations of the patients for less invasive approach avoiding sternotomy, we changed our policy and started to perform the transcervical-bilateral video-assisted thoracoscopic surgery (VATS) technique, with elevation of the sternal manubrium and introduction of three ports on each side of the chest as described by Novellino et al. (3). Soon, we found that this technique was not comfortable for us, in part due to our small experience in VATS surgery, at that time. We decided to change our approach by adding the subxiphoid approach with double elevation of the sternum from the side of the manubrium and the lower angle of the sternum. Initially, we tried the subxiphoid longitudinal midline incision, but very soon it was replaced with the transverse incision, which provided much better access to the mediastinum. Finally, our approach consisted of the collar incision in the neck combined with bilateral one-port thoracoscopy and the subxiphoid incision with double elevation of the sternum provided with the modified Rochard frame (Aesculap-Chifa) (4). We called this procedure the transcervical-subxiphoid-videothoracoscopic “maximal” thymectomy. Our aim was to remove maximally the whole thymus with the surrounding fatty tissue of the lower neck and the anterior and middle mediastinum. We tried to perform thymectomy in the same radical way as was described by Jaretzki et al. (5). Initially, for several years most of the procedure was performed mainly through the transcervical incision, with dissection of both laryngeal recurrent nerves, the vagus nerves, the upper poles of the thymus, the lower thyroid and the thymic veins, removal of the fatty tissue from the right paratracheal space (called by us “the aorta-caval groove”) and the fatty tissue of the aorta-pulmonary window. The upper part of the thymus was dissected from the pericardium. The subxiphoid approach was used for dissection of the lower part of the thymus from the pericardium and for removal of the epiphrenic fat pads bilaterally. Both pleural cavities were widely opened and the sheets of pleura were removed with the whole specimen en-block. Subsequently, our technique of thymectomy was modified with introduction of the “two team approach”, with two surgical teams working simultaneously—one from the transcervical and theother from the subxiphoid side (6). This policy helped us to reduce the operating time from 2.5–3 hours to 1.5–2 hours. We operated on 401 patients with use of this technique (390 patients operated for nonthymomatous myasthenia gravis (MG), 7 patients for thymomas and 4 for rethymectomies (in the period 1.9.2000–31.12.2015).
The next modification of our technique of thymectomy was the omission of the transcervical incision to reduce the invasiveness and for better cosmesis. This technique was called the subxiphoid-right VATS extended thymectomy and initially, was used for resection of thymomas (7). Subsequently, this technique was modified by adding a single left VATS port and was used for thymectomy for nonthymomatous MG and for rethymectomies, besides that of thymomas. This technique was described as the subxiphoid VATS extended thymectomy (8). In our last modification the intercostal VATS ports were replaced with bilateral single ultra-long bariatric laparoscopy ports introduced subcostally to the pleural cavities, through the insertions of the diaphragm to the chest wall, without violation of the peritoneal cavity. This new approach, called the subxiphoid-subcostal-VATS extended thymectomy will be described for the first time in this article. We started to use it from 16.8.2013. The Table 1 presents the numbers of patients operated on with use of and the subxiphoid-bilateral VATS extended thymectomy.
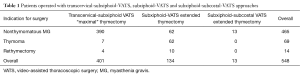
Full table
Patient selection and workup and pre-operative preparation
All patients with nonthymomatous MG are the candidates for this kind of procedure. In case of the advanced stage III thymomas the transsternal approach is preferred (9-11). In case of nonthymomatous MG the operation is proposed primarily to patients in the MGFA class I–IIIb (mild to moderate ocular, bulbar and extremities’ muscles affected) (12). In case of severe MG the operation is postponed until the patient’s clinical improvement after preoperative preparation with steroids, immunosuppressive drugs, plasmapheresis or immunoglobulins.
Equipment preference card
- The modified Rochard frame with two hooks;
- Bi-clamp, Harmonic knife or LigaSure;
- The Yankauer suction tube;
- The Cameleon videothoracoscope (Carl Storz);
- Standard VATS instruments;
- The extra-long bariatric laparoscopy ports.
Surgical technique
Preparation
The patient was positioned supine on the operating table with a roll placed beneath the thoracic spine to elevate the chest and to hyperextend the patient’s neck. Under general anaesthesia an endobronchial tube was inserted to conduct selective lung ventilation during the latter part of the procedure.
A transverse 5 cm subxiphoid incision was made above the xiphoid process. The subcutaneous tissue and the medial parts of the rectus muscles were cut near the insertions to the costal arches. The xiphoid process was removed. Selective left lung ventilation was started resulting in the collapse of the right lung. The anterior mediastinum was opened from below the sternum. A sternal retractor connected to the traction frame (Rochard bar, Aesculap-Chifa, Nowy Tomysl, Poland) was placed under the sternum, which was elevated to facilitate access to the anterior mediastinum from below (Figure 1). The single 10 mm extra-long bariatric laparoscopy ports were inserted to the right chest cavity for videothoracoscope (VATS) and subsequently for chest tube. To avoid injury of the peritoneum and entrance to the abdominal cavity a special technique of the port insertion was used (Figure 2). The first step was to introduce the Cameleon thoracoscope supplied with a very wide range of view enabling to view the insertion of the diaphragm in the area the port is going to be introduced. Subsequently the Yankauer suction tube is used to stretch the diaphragm by pressure in the direction of the spine. Therefore, the introduction of the port is made under control of VATS. The whole dissection was performed through the subxiphoid incision under control of a videothoracoscope inserted alternatively to the right and left pleural cavities.


The right mediastinal pleura was cut near the sternal surface up to the level of the right internal thoracic vein, which was left intact with bipolar cautery (Bi-Clamp, ERBE). Alternatively, such devices as a harmonic knife, LigaSure or vascular clips can be used to secure the vessels throughout the procedure (Figure 3). After dissection of the mediastinal tissue from the inner surface of the sternum a 2−3 mm puncture was performed over the sternal notch and a single-tooth hook was inserted percutaneously under the sternal manubrium (Figure 4). The second hook improved exposure of the superior mediastinal and the lower neck regions facilitating considerably performance of the procedure and enabling visualization of the whole upper poles of the thymus and the lower part of the thyroid. The prepericardial fat and the right epiphrenic fat pads were dissected from the pericardium and diaphragm (Figure 5). Dissection of the prepericardial fat containing the thymus gland proceeded upwards under control of thoracoscope in en bloc fashion, without any attempt to dissect the thymus gland with thymoma separately. The right phrenic nerve was a margin of dissection. The dissection of the thymus proceeded along the left innominate vein with closure with vascular clips and division of the thymic veins, until the left internal thoracic vein (left mammary vein) was visualized. The left mediastinal pleura was opened at the relatively early stage of dissection, enabling the manoeuvre of transferring of the dissected specimen obscuring plane of dissection from the right to the left pleural cavity (Figure 6). This manoeuvre facilitated dissection substantially due to improved exposure of the rest of the thymus. Dissection proceeded cranially with closure and division of the lower thyroid veins, performed in the same way as in the case of the thymic veins. Further dissection proceeded along the thymic poles until the lower part of the thyroid was clearly visualized (Figure 7). The specimen is dissected from the right and the left sides until the thyro-thymic ligaments are the sole attachments from the cranial side. At this point the upper poles were divided close to the thyroid. After dissection such structures as the innominate, the right carotid arteries and the trachea were clearly visualized. The liberated upper poles of the thymus were grabbed and pulled caudally enabling dissection of the thymus from the pericardium. A single ultra-long bariatric laparoscopic port was inserted subcostally to the left pleural cavity, in the same way as it was done on the right side. Dissection of the specimen along the left phrenic nerve was performed, the same as was done on the right side. The specimen containing the thymus and the adipose tissue was placed in a plastic bag and removed through the subxiphoid incision (Figure 8). Dissection of the aorta-pulmonary window was completed, finally (Figure 9). Haemostasis was checked and single chest tubes were inserted into both pleural cavities through the incisions made for insertion of the ports. Ventilation of both lungs was resumed. The subxiphoid incision was closed in the standard manner, a puncture incision was closed with a single 5/0 suture, which was replaced with a peristrip on the next day. The patient was extubated immediately after the operation.




Generally, the dissection of the neck area performed during the subxiphoid VATS extended thymectomy and the subxiphoid subcostal VATS extended thymectomy is less extensive than in the transcervical-subxiphoid-VATS approach. Therefore, we describe the techniques without a cervical incision as the extended, contrary to the previous technique called as “the maximal”. Nevertheless, the differences of extensiveness between the techniques with and without the transcervical incisions are probably slight. The reason to replace a intercostal incision for the subcostal one for insertion of the ports is due to a possible reduction of the postoperative pain. Our initial unpublished experience with the subcostal approach for thymectomy and VATS pulmonary lobectomy suggested that the subcostal incision was probably less painfull than the intercostal one. Currently, we are conducting a prospective randomized trial comparing the subxiphoid-bilateral VATS thymectomy with the subxiphoid-subcostal bilateral VATS thymectomy, in regard to the amount of the postoperative pain and reduction of the spirometric parameters. The closure of accrual of all patients for the completion of the study and the presentation of the results are expected in the next year.
The subxiphoid-bilateral VATS approach with elevation of the sternum with two hooks was used in 147 patients (62 patients operated on for thymomas, 75 patients for nonthymomatous MG and 10 for rethymectomies) in the period 1.1.2009–30.3.2016. There was no mortality and 3.4% morbidity. The mean operative time was 109.1 min (range, 75–150 min). The dimensions of the largest thymoma removed completely with this technique were 13 cm × 10 cm ×5 cm. The subxiphoid-subcostal-VATS thymectomy was performed in 13 patients with nonthymomatous MG in the period 16.8.2013–30.3.2016.
Post-operative management
Generally, a patient is extubated immediately after the operation. Steroids and/or immunosuppressive drugs are started soon after the operation. The anticholinesterase drugs given in the preoperative doses are resumed when the clinical symptoms of MF recur, which may happen after a variable period of time. Generally, the chest tubes are removed on the first or second postoperative day and the patients are discharged on the 4–7th postoperative day.
Tips, tricks and pitfalls
- The subxiphoid incision should be performed just below the junction of the lower angle of the sternum. The length of the incision depends on the patients’ body habitus—in case of slim patients 3 cm could provide an adequate approach instead of the length of 5 cm, which is usually performed in the medium body habitus patients;
- Generally, we start dissection from the right pleural cavity with completion of dissection in left one;
- After dissection of the mediastinum from the posterior surface of the sternum the mediastinal structures are pressed posteriorly towards the spine, with the Yankauer suction tube to protect these structures from injury during percutaneous insertion of the second sternal hook elevating the sternal manubrium;
- To avoid injury of the peritoneum and entrance to the abdominal cavity a special technique of the port insertion was used. The first step was to introduce the Cameleon thoracoscope supplied with a very wide range of view enabling to view the insertion of the diaphragm in the area the port is going to be introduced. Subsequently the Yankauer suction tube is used to stretch the diaphragm by pressure in the direction of the spine. Therefore, the introduction of the port is made under control of VATS;
- The next step is dissection of the right epiphrenic fat pad from the right dome of the diaphragm and the pericardium. Dissection of the specimen containing the whole thymus gland is proceeded in the cephalad direction. In case of obese patients and especially in thymomas it is useful to open the mediastinal pleura to transfer the specimen to the contralateral left pleural cavity. This maneuver gives the clear view of the plane of dissection facilitates dissection of the specimen from the pericardium;
- During dissection on the right it is useful to rotate an operating table to the right and to rotate it in the opposite direction during dissection on the left side;
- Dissection of the area cranial to the left innominate vein is the most difficult part of the procedure. The aim is to reach and visualize of lower poles of the thyroid gland to remove completely the upper poles of the thymus and the surrounding fatty tissue. The innominate artery, right and left carotid arteries and the trachea should be clearly dissected. This can be achieved with the simultaneous use of the bipolar cautery (or harmonic knife or LigaSure) and the Yankauer suction tube, which is used to dissect and retract tissue. Avoidance of injury of the left recurrent nerve might occur during dissection in the area located on the left side of the trachea;
- Dissection and removal of the fatty tissue from the aorta-pulmonary window is done separately after extraction of specimen from the chest.
Possible future modifications
- Uniportal subxiphoid technique with avoidance of the additional incision for ports;
- The use of CO2 insufflation. It would be possible if the single incision laparoscopic port (SILS port) is used as was described by Suda et al. (22).
Acknowledgements
All Authors declare no conflict of interest. We are grateful to Mr. Bogdan Dziadzio for preparation of the drawings and to Mr. Michael Clark to reviewing the manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethical committee (No. KB/430-37/14) and written informed consent was obtained from all patients.
References
- Bulkley GB, Bass KN, Stephenson GR, et al. Extended cervicomediastinal thymectomy in the integrated management of myasthenia gravis. Ann Surg 1997;226:324-34; discussion 334-5. [Crossref] [PubMed]
- Zieliński M, Kuzdzal J, Szlubowski A, et al. Comparison of late results of basic transsternal and extended transsternal thymectomies in the treatment of myasthenia gravis. Ann Thorac Surg 2004;78:253-8. [Crossref] [PubMed]
- Novellino L, Longoni M, Spinelli L, et al. "Extended" thymectomy, without sternotomy, performed by cervicotomy and thoracoscopic technique in the treatment of myasthenia gravis. Int Surg 1994;79:378-81. [PubMed]
- Zieliński M, Kuzdzał J, Szlubowski A, et al. Transcervical-subxiphoid-videothoracoscopic "maximal" thymectomy--operative technique and early results. Ann Thorac Surg 2004;78:404-9; discussion 409-10. [Crossref] [PubMed]
- Jaretzki A 3rd, Bethea M, Wolff M, et al. A rational approach to total thymectomy in the treatment of myasthenia gravis. Ann Thorac Surg 1977;24:120-30. [Crossref] [PubMed]
- Zielinski M, Hauer L, Hauer J, et al. Comparison of complete remission rates after 5 year follow-up of three different techniques of thymectomy for myasthenia gravis. Eur J Cardiothorac Surg 2010;37:1137-43. [Crossref] [PubMed]
- Zielinski M, Czajkowski W, Gwozdz P, et al. Resection of thymomas with use of the new minimally-invasive technique of extended thymectomy performed through the subxiphoid-right video-thoracoscopic approach with double elevation of the sternum. Eur J Cardiothorac Surg 2013;44:e113-9; discussion e119.
- Zieliński M, Rybak M, Wilkojc M, et al. Subxiphoid video-assisted thorascopic thymectomy for thymoma. Ann Cardiothorac Surg 2015;4:564-6. [PubMed]
- Masaoka A, Monden Y, Nakahara K, et al. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92. [Crossref] [PubMed]
- Koga K, Matsuno Y, Noguchi M, et al. A review of 79 thymomas: modification of staging system and reappraisal of conventional division into invasive and non-invasive thymoma. Pathol Int 1994;44:359-67. [Crossref] [PubMed]
- Detterbeck FC, Nicholson AG, Kondo K, et al. The Masaoka-Koga stage classification for thymic malignancies: clarification and definition of terms. J Thorac Oncol 2011;6:S1710-6. [Crossref] [PubMed]
- Jaretzki A 3rd, Barohn RJ, Ernstoff RM, et al. Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Ann Thorac Surg 2000;70:327-34. [Crossref] [PubMed]
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Subxiphoid incision, elevation of the sternum, opening of the right mediastinal pleura. Asvide 2016;3:502. Available online: http://www.asvide.com/articles/1277
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Introduction of the video-assisted thoracoscopic surgery (VATS) port through the subcostal incision to the right pleural cavity. Asvide 2016;3:503. Available online: http://www.asvide.com/articles/1278
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Dissection of the mediastinal tissue from the sternum. Asvide 2016;3:504. Available online: http://www.asvide.com/articles/1279
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Introduction of the upper sternal hook. Asvide 2016;3:505. Available online: http://www.asvide.com/articles/1280
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Dissection of the right epiphrenic fat pad from the diaphragm and the pericardium. Asvide 2016;3:506. Available online: http://www.asvide.com/articles/1281
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Opening of the left mediastinal pleura, transfer of the specimen to the left pleural cavity. Asvide 2016;3:507. Available online: http://www.asvide.com/articles/1282
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Dissection of the right and left lobes of the thyroid gland, the lower thyroid vein, the trachea and the thymic vein. Asvide 2016;3:508. Available online: http://www.asvide.com/articles/1283
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Dissection of the specimen from the left phrenic nerve and removal of the specimen in the bag. Asvide 2016;3:509. Available online: http://www.asvide.com/articles/1284
- Zieliński M, Rybak M, Solarczyk-Bombik K, et al. Dissection of the aorta-pulmonary window. Asvide 2016;3:510. Available online: http://www.asvide.com/articles/1285
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
Cite this article as: Zieliński M, Rybak M, Solarczyk-Bombik K, Wilkojc M, Czajkowski W, Kosinski S, Fryzlewicz E, Nabialek T, Szolkowska M, Pankowski J. The Zakopane Pulmonary Hospital experience on subxiphoid thymectomy. J Vis Surg 2017;3:2.


