Robot-assisted lobectomy for lung cancer in the presence of intraoperatively discovered broncho-vascular anomalies affecting right upper and middle lobes
Introduction
Surgeons performing video and robotic-assisted thoracic surgery for lung cancer should have detailed knowledge of anatomical variations of pulmonary arteries, veins and bronchial branching to avoid inadvertent ligations and vascular injuries. In this case report, we describe the intraoperative management of a broncho-vascular variation, discovered during robotic lobectomy, consisting of the presence of a right upper and middle lobes supplied by a common bronchus and pulmonary vein, and an anomalous course of the pulmonary artery (PA).
Case presentation
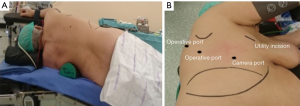
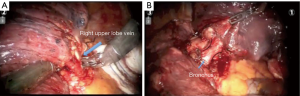
A 76-year-old woman, never smoker, was scheduled for robotic right lung upper lobectomy after CT had revealed a partially solid peripheral lung nodule, 1.5 cm diameter, PET positive (SUV 1.5), diagnosed as adenocarcinoma. The anomaly was not observed on CT, and a bronchoscopy was not performed (stage IA). The procedure was performed under general anaesthesia. One-lung ventilation achieved by use of a double-lumen endotracheal tube. Patience was placed in left lateral decubitus, with the hips flexed and secured by fixing the pelvis. We proceeded to perform a four incisions approach. A 3-cm utility incision was performed in the fourth intercostal space anteriorly. Camera port was placed in the seventh intercostal space along the axillary line, and a 30-degree three-dimensional endoscope was then inserted to explore the thoracic cavity. Under direct vision, an 8-mm incision was performed in the eighth intercostal space (posterior axillary line) and the fourth 8-mm incision was performed in the auscultatory triangle. The fourth incision allows lung retraction and hence better field exposure (Figure 1). Intraoperative inspection of the lung showed the absence of the middle lobe vein and absence of a fissure between the upper and intermediate lobes. The isolation of the PA exposed two large PA branches in a single lobe, without evidence of a separate PA branch to the middle lobe. The upper lobe vein was parted with a vascular stapler exposing a single common bronchus to the single anomalous lobe (Figure 2). The course of the main PA tracked the course the left main PA. After the intraoperative review of available imaging, the preoperative CT confirmed the absence of the right upper bronchus. Therefore, the surgeons decided to complete the upper lobectomy robotically (Figure 3). Conversion to open surgery was not required. The postoperative course was regular. The patient was discharged on the fourth postoperative day. The definitive histological diagnosis was adenocarcinoma of the lung pT1a N0 M0.

Discussion
Current literature shows that robotic lobectomy is a safe and feasible procedure in experienced surgeons (2,3). The incidence of severe intraoperative complications is low but potentially life-threatening (4). To avoid catastrophic complications, a preoperative knowledge of vascular and bronchial anomalies is paramount. In the preoperative workup for clinical T1 N0, we do not routinely perform an inspective bronchoscopy. In the case showed, a preoperative bronchoscopy would have shown both the absence of a separated middle bronchus, and the presence of a single common bronchus related to a single anomalous lobe. This more thorough preoperative examination would allow an easier, and safer dissection of the hilar structure is reducing the risk of inadvertent vascular or bronchial ligations (5,6). Postoperative revision of the CT scans revealed the anomalous course of the PA, but the absence of middle lobe PA branch was not detectable.
Conclusions
This type of anomaly of the course of the right main PA is exceptional and not described in the literature. The vascular and bronchial division of the right upper and middle lobe mimicked the anatomy of left upper lobe and lingula, with a common pulmonary vein and bronchus without a distinct pulmonary artery branch for the middle lobe. A preoperative evaluation of the presence of potential anatomical anomalies is recommended to prevent vascular injuries during minimally invasive procedure avoiding the necessity to convert to an open procedure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Pardolesi A, Bertolaccini L, Solli P, et al. Surgical case description. Asvide 2016;3:486. Available online: http://www.asvide.com/articles/1261
- Park BJ, Flores RM, Rusch VW. Robotic assistance for video-assisted thoracic surgical lobectomy: technique and initial results. J Thorac Cardiovasc Surg 2006;131:54-9. [Crossref] [PubMed]
- Cerfolio RJ. Total port approach for robotic lobectomy. Thorac Surg Clin 2014;24:151-6. v. [Crossref] [PubMed]
- Flores RM, Ihekweazu U, Dycoco J, et al. Video-assisted thoracoscopic surgery (VATS) lobectomy: catastrophic intraoperative complications. J Thorac Cardiovasc Surg 2011;142:1412-7. [Crossref] [PubMed]
- Desir A, Ghaye B. Congenital abnormalities of intrathoracic airways. Radiol Clin North Am 2009;47:203-25. [Crossref] [PubMed]
- Castañer E, Gallardo X, Rimola J, et al. Congenital and acquired pulmonary artery anomalies in the adult: radiologic overview. Radiographics 2006;26:349-71. [Crossref] [PubMed]
Cite this article as: Pardolesi A, Bertolaccini L, Solli P, Novellis P, Veronesi G. Robot-assisted lobectomy for lung cancer in the presence of intraoperatively discovered broncho-vascular anomalies affecting right upper and middle lobes. J Vis Surg 2016;2:175.


