Uniportal subxiphoid video-assisted thoracoscopic bilateral segmentectomy for synchronous bilateral lung adenocarcinomas
Introduction
Synchronous, bilateral, early-stage primary non-small cell lung cancers (NSCLC) are not uncommon and an aggressive surgical approach may offer the greatest chance of long-term survival (1). However, the decision to undertake bilateral concomitant surgical resection should be made carefully, taking into consideration the higher risk of post-operative morbidity and mortality related to performing bilateral lung procedures in a single operation. In these cases, a minimally invasive approach could lead to a reduction in post-operative complication risks without compromising the oncological result. We present a case of bilateral synchronous NSCLC successfully treated by uniportal subxiphoid video-assisted thoracic surgery (SVATS) bilateral segmentectomies and discuss our experience developing the SVATS technique.
Clinical summary
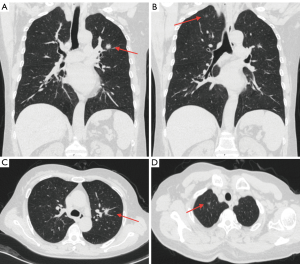
A 60-year-old female presented with a month long history of a persistent cough. Preoperative high-resolution computed tomography revealed a 1.6 cm solid lesion located at the confluence of the three apical segments of the left upper lobe and a 0.8cm ground glass opacity lesion in the apical segment of the right upper lobe. There was no evidence of lymph node involvement (Figure 1). Bronchoscopically-guided biopsies failed to reveal the nature of the lesions. As there were no surgical contra-indications, concomitant bilateral segmentectomies via a uniportal subxiphoid incision (SVATS) were planned.
Surgical technique
Operating room set up
After induction of general anesthesia and intubation with a double-lumen endotracheal tube, the patient was positioned in the right semidecubitus position at a 60° angle to the table.
The standard set-up of the operating room consisted of a single monitor, positioned cranially, above the head of the patient. The first surgeon and the scrub nurse are positioned on the ventral side of the patient with the assistant surgeon on the opposite side.
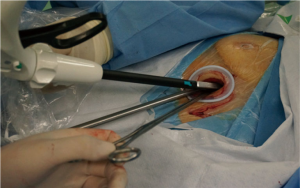
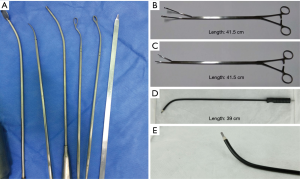
A 10-mm, 30° angled thoracoscope and dedicated instruments designed for SVATS (Shanghai Medical Instruments Group Ltd.) were used during the operation (Figures 2,3).
Creation of the subxiphoid single port
A 4-cm longitudinal incision was made over the subxiphoid area, the xiphoid process was cut and blunt dissection was carried out under the sternum to reach the right pleural cavity. A wound protector was placed to provide optimal exposure.
Right upper lobe upper segmentectomy (Figure 4)
The lung was retracted posteriorly and inferiorly using a specifically designed lung grasper. Dissection was performed along the border of the superior pulmonary vein and around the superior part of the hilum, inferior to the azygos vein. The apical branch of the superior pulmonary vein was dissected, ligated with a non-absorbable suture, and divided using the LigaSure device.
The mediastinal trunk of the pulmonary artery was identified and after a further distal dissection, A1 and A3 branches were visualized. The upper segment artery (A1) was ligated and divided in the same manner as the apical vein branch.
The apical segmental bronchus was then identified and was divided using a stapler. The intersegmental plane was identified by ventilating the lung and then divided using staplers. The resected apical segment was extracted using an endobag. Lymph node sampling was then carried out for stations 12R, 11R, 4, and 2.
Left upper lobe apical trisegmentectomy (Figure 4)
After the right side lung resection, the patient was rotated and re-positioned in the left semidecubitus position at a 60o angle in preparation for the left sided resection.
Using the same 4-cm longitudinal subxiphoid incision, blunt dissection was performed to reach the left pleural cavity and the wound protector adjusted to provide optimal access.
The lung was retracted posterolaterally and dissection carried out along the superior border of the superior pulmonary vein until the descending aorta was visualized. Following inspection of the superior pulmonary vein the veins draining the three superior segments were identified, isolated and transected using a stapler. The lingular vein was identified and spared.
The lung was then re-positioned with postero-inferior traction and the anterior trunk was dissected and transected using a stapler. The lymph nodes on the left upper lobe bronchus were excised to improve dissection of the plane between the bronchus and the posterior ascending artery. This artery was then ligated using a non-absorbable suture and transected using the LigaSure device.
The bronchus was dissected towards the lung parenchyma and the upper bronchial division transected using a stapler. Special care was taken to ensure preservation of the lingular bronchus.
The lung was ventilated to visualise better the fissure between the apical trisegment and the lingula and this was then divided using multiple staplers, taking care not to injure the lingular artery.
The lung specimen was extracted through the subxiphoid incision and lymph node sampling performed for stations 5, 6, 7, 9L, 11L,12L.
Prior to closure, a 28F straight chest tube was inserted in each pleural cavity via the subxiphoid incision. The total operative time was 180 minutes, and the total blood loss was 150 mL.
Results
Postoperative results
The patient was extubated in the operating room. She was then transferred to the post-operative intensive care unit where she remained stable and after 16 hours she was transferred to the surgical ward.
The post-operative course was uneventful. The drains were removed on the forth post-operative day and the patient discharged on the fifth post-operative day.
The intensity of post-operative pain was evaluated every 8 hours by means of a visual analog scale, which ranged from 0 (painless) to 10 (worst pain ever experienced). The maximal mean pain score at rest was 4 (immediately post-procedure) and this declined steadily to 0 by the 2nd post-operative day. The pain was limited to the subxiphoid area and did not restrict mobility or routine activities of daily living.
Pathological results
Histopathology revealed invasive adenocarcinoma in the left-sided lesion and an adenocarcinoma in situ on the right. All the sampled lymph nodes were negative for malignancy.
Discussion
As shown by Jung et al. concomitant surgical treatment for synchronous, multiple, bilateral NSCLC can offer the greatest chance of long-term survival (1). Also, recent meta-analyses have shown that segmentectomy may be considered an oncologic equivalent treatment to lobectomy for NSCLC sized 20 mm or smaller (3,4). In this case, performing bilateral uniportal SVATS segmentectomies achieved the oncological goal of simultaneous, anatomically-complete, bilateral lesion resection with reduced peri-operative morbidity compared to conventional approaches.
Uniportal video-assisted thoracic surgery (VATS) through an intercostal space has been shown to have reduced post-operative rates of acute and chronic pain, allodynia, hypaesthesia and numbness compared to the conventional multiportal VATS approach (5). Patients undergoing a uniportal procedure, therefore report better quality of life post-lung resection than the multiportal patients (5). However, as any intercostal approach still involves an element of rib spreading and potential damage to the intercostal neurovascular bundles, these complications are not completely eradicated (5). Uniportal SVATS avoids any intercostal approach and so reduces the risk of damage to the neurovascular bundle, theoretically, improving upon the benefits of uniportal VATS. Furthermore, uniportal SVATS makes bilateral procedures possible through a single incision (6) and therefore makes this a reasonable approach to consider in patients with bilateral, synchronous tumours.
Previously, uniportal SVATS had only been described for non-anatomical lung resection or upper lobectomies and the reported clinical experience and evidence for this technique is still sparse (6-8). In Shanghai Pulmonary Hospital, after extensive experience in multiportal and uniportal VATS, we started the uniportal SVATS program for lobar and sublobar anatomical lung resections in September 2014 and our preliminary results showed the feasibility and the safety of the subxiphoid approach (9-11).
The subxiphoid approach presents some additional challenges and limitations compared to the standard VATS approach; however, with experience we have overcome several of the initial technical difficulties and these are described below:
- Access to the posterior anatomy can be more difficult using the subxiphoid approach but with appropriate retraction of the lung and optimization of the thoracoscope position it is possible to achieve good exposure of almost every portion of the chest cavity;
- At the beginning of our SVATS programme we were able to perform just lymph node sampling but with experience we gradually increased the number of lymph nodes dissected. We are now able to perform a systematic lymph node dissection with removal of lymph nodes from at least 3 N2 stations (as per the IASLC/Mountain classification). Dissection of the station 7 lymph node is particularly difficult and has been one of the toughest elements in our ‘subxiphoid learning curve’;
- Working on the left pleural cavity can be very challenging, especially in case of cardiomegaly, because the cardiac pulsation is transmitted to the instruments. Another issue, when working on the left side, is that the compression of the heart can lead to intra-operative arrhythmias and hypotension;
- Despite, overcoming several technical challenges of the subxiphoid approach, there remain several segments that are not amenable to resection via SVATS and that require a more conventional VATS technique. In particular, S2 and S6 segmentectomies on the left and S9 and S10 bilaterally.
Conclusions
In our experience uniportal SVATS offers post-operative recovery benefits that over conventional intercostal uniportal VATS. Whilst there is a significant learning curve for this SVATS technique, we believe that the benefits for selected patients make this an important approach for thoracic surgeons to develop. In conclusion, this case highlights the feasibility of uniportal SVATS bilateral segmentectomy as a minimally invasive treatment option in patients with bilateral, synchronous NSCLC.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Jung EJ, Lee JH, Jeon K, et al. Treatment outcomes for patients with synchronous multiple primary non-small cell lung cancer. Lung Cancer 2011;73:237-42. [Crossref] [PubMed]
- Aresu G, Weaver H, Jiang L, et al. Uniportal video-assisted thoracic surgery (VATS) subxiphoid right upper apical segmentectomy and left upper trisegmentectomy. Asvide 2016;3:456. Available online: http://www.asvide.com/articles/1229
- Bao F, Ye P, Yang Y, et al. Segmentectomy or lobectomy for early stage lung cancer: a meta-analysis. Eur J Cardiothorac Surg 2014;46:1-7. [Crossref] [PubMed]
- Zhang L, Li M, Yin R, et al. Comparison of the oncologic outcomes of anatomic segmentectomy and lobectomy for early-stage non-small cell lung cancer. Ann Thorac Surg 2015;99:728-37. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i37-41. [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [Crossref] [PubMed]
- Aresu G, Wu L, Lin L, et al. The Shanghai Pulmonary Hospital subxiphoid approach for lobectomies. J Vis Surg 2016;2:135. [Crossref]
- Song N, Zhao DP, Jiang L, et al. Subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) for lobectomy: a report of 105 cases. J Thorac Dis 2016;8:S251-7. [PubMed]
- Hernandez-Arenas LA, Lin L, Yang Y, et al. Initial experience in uniportal subxiphoid video-assisted thoracoscopic surgery for major lung resections. Eur J Cardiothorac Surg 2016. [Epub ahead of print]. [Crossref] [PubMed]
Cite this article as: Aresu G, Weaver H, Wu L, Lin L, Sponga S, Jiang G, Jiang L. Uniportal subxiphoid video-assisted thoracoscopic bilateral segmentectomy for synchronous bilateral lung adenocarcinomas. J Vis Surg 2016;2:170.