Uniportal video-assisted thoracic surgery lobectomy using a novel perfused ex vivo simulation model
Introduction
Minimally invasive procedures have increased their use in thoracic surgery because of less postoperative pain and faster recovery; being the video assisted thoracic surgery the gold standard for early stage lung cancer surgery (1). Teaching procedures usually follows the classic Halsted methodology of “See one, do one, teach one” (2). However, the increase in legal constraints related to patient safety in addition to residents working hours restrictions, has decreased the acquisition of experience related to clinical cases (3,4). Medical simulation emerges as a complement to traditional teaching and as a powerful educational tool which allows homogeneous training in a controlled and safe environment (5,6). The Universidad Catolica de Chile Simulation Center has become an international reference in Latin America in the training of minimally invasive surgeons with hi fidelity and low-cost simulation models, shortening learning curves and decreasing complication rates in surgical procedures (7-10).
Universidad Catolica de Chile uniportal video-assisted thoracic surgery (VATS) simulation model
The swine is a validated model in thoracic surgery training and it has been used both in a live (11) and ex vivo model (12). There are no reports in the English literature about a perfused ex vivo model.
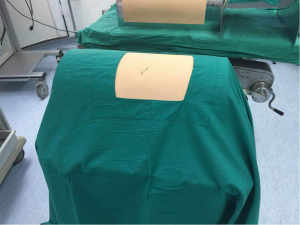
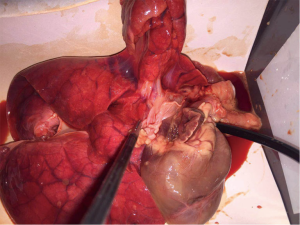
We developed a low cost and hi fidelity model using an ex vivo in bloc heart and lung specimen from a swine (Figures 1,2). The swine was previously used in a non-thoracic experiment, so we extracted the lung and heart for this ex vivo based model to reduce animal use. The cost of the whole model is 70 USD and it can be reused many times changing the ex vivo tissue.
This model has been used for open surgery simulation (thoracotomy) and minimally invasive surgery. The proposed model was validated during the ALAT 2016 annual congress uniportal vats course by Dr. Diego Gonzalez-Rivas, thoracic surgeon who was invited to participate with informed consent document (Figure 3) (13).
Model and video description
As in a traditional uniportal human surgery, the model has a 4 cm utility incision. A 30° 10 mm camera was used in the posterior aspect of the incision. First, the left superior lobe is retracted posteriorly for hilum exposure. The anterior structure is the superior pulmonary vein. After opening the mediastinal pleura, dissection of the superior pulmonary vein is performed with blunt dissection and with an energy device. Section of the vein is made with a vascular endo-stapler. This exposes the main pulmonary artery. The next step is to identify the arterial branches for the superior lobe and divide them with a vascular stapler. To finalize, the upper lobe bronchus is dissected and then cut with a medium thickness endo-stapler.
In the video, the setting of the surgeon and his assistant is shown in a comparable fashion to a human uniportal vats surgery (Figures 4,5).

By pulmonary artery cannulation, the lung can be perfused with simulated blood allowing a more accurate vascular dissection.
In order to demonstrate how well the system is perfused, a continuous bleeding secondary to an intentional arterial cut was shown. As this is a simulated blood perfused model it allows the operator to dissect the vessels in a more realistic setting (the vessels are not collapsed) and to see bleeding in case of any damage.
Conclusions
A low cost and hi fidelity perfused uniportal VATS model was validated by an expert thoracic surgeon in uniportal VATS. This model may help reduce the costs and animal use associated to this high complexity surgery.
Acknowledgements
Dr. Diego Gonzalez-Rivas for using the model.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-313S.
- Osborne MP. William Stewart Halsted: his life and contributions to surgery. Lancet Oncol 2007;8:256-65. [Crossref] [PubMed]
- Aggarwal R, Darzi A. Simulation to enhance patient safety: why aren't we there yet? Chest 2011;140:854-8. [Crossref] [PubMed]
- Reznick RK, MacRae H. Teaching surgical skills--changes in the wind. N Engl J Med 2006;355:2664-9. [Crossref] [PubMed]
- Corvetto M, Bravo MP, Montaña R, et al. Simulation in medical education: a synopsis. Rev Med Chil 2013;141:70-9. [Crossref] [PubMed]
- Harris P, Snell L, Talbot M, et al. Competency-based medical education: implications for undergraduate programs. Med Teach 2010;32:646-50. [Crossref] [PubMed]
- Boza C, Varas J, Buckel E, et al. A cadaveric porcine model for assessment in laparoscopic bariatric surgery--a validation study. Obes Surg 2013;23:589-93. [Crossref] [PubMed]
- Castillo R, Buckel E, León F, et al. Effectiveness of learning advanced laparoscopic skills in a brief intensive laparoscopy training program. J Surg Educ 2015;72:648-53. [Crossref] [PubMed]
- León Ferrufino F, Varas Cohen J, Buckel Schaffner E, et al. Simulation in laparoscopic surgery. Cir Esp 2015;93:4-11. [PubMed]
- Varas J, Mejía R, Riquelme A, et al. Significant transfer of surgical skills obtained with an advanced laparoscopic training program to a laparoscopic jejunojejunostomy in a live porcine model: feasibility of learning advanced laparoscopy in a general surgery residency. Surg Endosc 2012;26:3486-94. [Crossref] [PubMed]
- Tedde ML, Brito Filho F, Belmonte Ede A, et al. Video-assisted thoracoscopic surgery in swine: an animal model for thoracoscopic lobectomy training. Interact Cardiovasc Thorac Surg 2015;21:224-30. [Crossref] [PubMed]
- Meyerson SL, LoCascio F, Balderson SS, et al. An inexpensive, reproducible tissue simulator for teaching thoracoscopic lobectomy. Ann Thorac Surg 2010;89:594-7. [Crossref] [PubMed]
- Clavero JM. Single port training in Latin-America—first uniportal video-assisted thoracoscopic surgery masterclass in Santiago, Chile. J Vis Surg 2016;2:140. [Crossref]
- Avila R, Achurra P, Salas P, et al. Perfused video-assisted thoracic surgery model. Asvide 2016;3:368. Available online: http://www.asvide.com/articles/1137
Cite this article as: Avila R, Achurra P, Tejos R, Varas J, Solovera M, Salas P. Uniportal video-assisted thoracic surgery lobectomy using a novel perfused ex vivo simulation model. J Vis Surg 2016;2:155.