First non-intubated uniportal video-assisted pulmonary lobectomy in America
Introduction
The first video-assisted thoracic lobectomy in non-intubated patient in America was performed on 27th of September 2014 in Colombia, The National Cancer Institute in Bogotá received Dr. Diego González-Rivas visit to make it possible. In our country video-assisted thoracic surgery (VATS) surgery for lung resection has evolved so far in the last 16 years approximately, Initially using three or four ports, but in 2011 with the influence of Thomas D’Amico from Duke University (1) we were interested in switch to use just two ports, at that time the main cities around the country had successfully implemented the minimally invasive Thoracic surgery. With a unique training program, the transition from two ports to uniportal VATS was accelerated to the point that today thoracic surgeons trained in the past 2 years have taken on a daily basis this technique, some of them directly from open surgery (2). The way to single port was driven by the rapid educational work and publications around the world of Dr. Diego González-Rivas with a large number of procedures replicated in many countries with diverse health systems, populations and medical teams (3).
We present a case of uniportal VATS surgery in our institution with the cooperation of an anesthesiologist willing to do it, radiologists and nuclear physicians responsible for the radio guided location of the nodules (because its location seemed difficult by palpation), and surgeons in the company of Dr. González-Rivas. We describe the first lobectomy in non-intubated patient reported in America in a single port approach, with the same technical challenges than intubated patients but with less anesthetic time and a faster postoperative recovery (4,5).
Clinical case
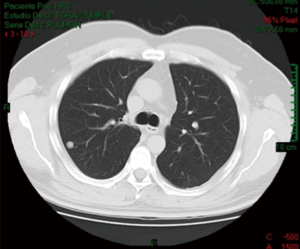
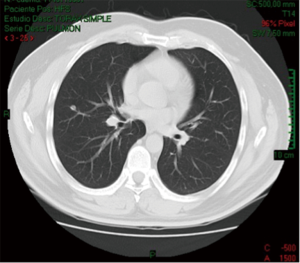
This patient is a 53-year-old man, with a history of papillary thyroid carcinoma classic pattern and follicular variant, initially staged T3N1BM0; surgically treated with total thyroidectomy with central lymph node dissection and left radical modified neck dissection, besides iodine therapy. In this patient follow-up 5 months later the tomography shows a 9.5 mm solid nodule in the posterior segment of the right upper lobe and another one 7.3 mm on the lateral segment of the middle lobe (Figures 1-3).
Non-intubated uniportal VATS middle lobectomy and wedge resection in the upper lobe, guided by scintigraphy to improve the location of the lesion were performed (7).
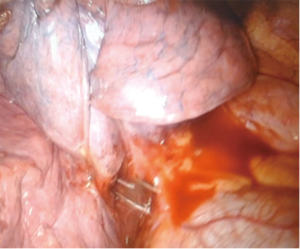
There was no problem with the lung collapse in the absence of double-lumen tube for anesthesia, because pneumothorax generated with the chest incision is sufficient to operate comfortably (Figure 4).
Surgical procedure
The patient is positioned in left lateral decubitus; the anesthesiologist provides oxygen by facemask to the patient and introduces an intranasal multi-perforated catheter in order to increase the O2 arterial pressure and to prevent upper airway obstruction (8,9). Intravenous anesthesia is administered and the surgeon makes a blockage in the fifth intercostal space with Bupivacaine.
A single incision in the 5th intercostal space was made, in few seconds pneumothorax occurs and then a 30 degree lens is inserted into the posterior end of the wound, below the thoracoscope we introduce the instruments for dissection and the staplers corresponding to each step of the procedure (Figure 5). Meanwhile the patient is breathing spontaneously without pain and the surgeon accompanies the subtle movements of the diaphragm.

In this case we performed at first the wedge resection of the upper lobe, verifying that the nodule is in the resected tissue by using the gamma probe which marked 1,500 accounts. After this step, we took the decision to make middle lobectomy because of the profound location of the second nodule and its radiological suspicion of malignancy.
With ultrasonic scalpel we dissected the middle lobe vein which is after divided with stapler, very calcified lymph nodes were resected enabling the corresponding artery dissection to be further divided with stapler too, the same procedure was made with the middle lobe bronchus; finally we completed de division of the cisure.
The lobe resected is extracted in a protective bag and at the end a chest tube is inserted and fixed in the posterior end of the incision (Figure 6).
Results
Even though the patient was overweight with slightly elevated diaphragm, we could make a safe procedure without bleeding or other intraoperative complications and also comfortable for the surgeon. From the viewpoint of anesthesia the patient went after surgery to a recovery unit, ten minutes later he was talking with us, in minimum pain; and from there he went to a room in our department ward, without intensive care unit necessity.
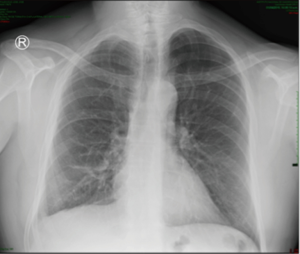
His radiological evolution went as usual and he was discharged on the third postoperative day after the chest tube removal. Chest X-ray and CT scan today show no new lesions (Figure 7).
Conclusions
Uniportal VATS is a surgical approach that we have adopted in our institution whenever is possible, and therefore we are open to the possibility of new developments in the art, that’s why it has been of great academic and practical interest to have made a middle lobectomy to a patient without endotracheal intubation, taught by the pioneer of the art and under strict security conditions in anesthesia.
This procedure the first reported in America, was replicated from others with similar results in several countries even in children (11); thanks to the collaboration between surgeons, anesthesiologists, radiologists, nurses and therapists and could be feasible in the future for our fragile oncologic population, with the advantage of the multidisciplinary approach that we can provide in our institution.
We believe that given the benefits in terms of spontaneous ventilation, fast recovery for the patient and the less anesthetic time, we could go on replicating the experience in selected patients.
Acknowledgements
Dr. Jorge Ramirez, Thoracic Surgery resident, for his great interest in this document.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Burfeind WR, D'Amico TA. Thoracoscopic lobectomy. Thoracic and Cardiovascular Surgery 2004;9:98-114.
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- González-Rivas D, Buitrago R. Case Report: Hilar mass resection using single port thoracoscopy with Dr. Diego González-Rivas. Thoracic Surgery 2013. Available online: https://thoracics.org/2013/09/02/case-report-hilar-mass-resection-using-single-port-thoracoscopy-with-dr-diego-gonzalez-rivas/
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Hung MH, Hsu HH, Cheng YJ, et al. Nonintubated thoracoscopic surgery: state of the art and future directions. J Thorac Dis 2014;6:2-9. [PubMed]
- Buitrago R, Serna A, González-Rivas D, et al. CT scan shows a 9.5 mm solid nodule in the posterior segment of the right upper lobe and another 7.3 mm nodule on the lateral segment of the middle lobe. Asvide 2016;3:345. Available online: http://www.asvide.com/articles/1114
- Boni G, Bellina CR, Grosso M, et al. Gamma probe-guided thoracoscopic surgery of small pulmonary nodules. Tumori 2000;86:364-6. [PubMed]
- Galvez C, Navarro-Martinez J, Bolufer S, et al. Benefits of awake uniportal pulmonary resection in a patient with a previous contralateral lobectomy. Ann Transl Med 2014;2:93. [PubMed]
- Irons JF, Martinez G. Anaesthetic considerations for non-intubated thoracic surgery. J Vis Surg 2016;2:61. [Crossref]
- Buitrago R, Serna A, González-Rivas D, et al. Wedge resection on the right upper lobe and middle lobectomy, with patient breathing spontaneously. Asvide 2016;3:346. Available online: http://www.asvide.com/articles/1115
- Hwang J, Min TJ, Kim DJ, et al. Non-intubated single port thoracoscopic procedure under local anesthesia with sedation for a 5-year-old girl. J Thorac Dis 2014;6:E148-51. [PubMed]
Cite this article as: Buitrago R, Serna A, González-Rivas D, Beltrán R, Palacio CM, Parades P, Beltrán J. First non-intubated uniportal video-assisted pulmonary lobectomy in America. J Vis Surg 2016;2:144.