The Shanghai Pulmonary Hospital subxiphoid approach for lobectomies
Background
Video-assisted thoracoscopic surgery (VATS), compared with open thoracotomy, has recognized benefits including lesser postoperative pain and the possibility of earlier mobilization (1-3).
However, patients undergoing VATS also complain of a moderate degree of acute postoperative pain and the incidence of chronic postoperative pain has been reported to be similar to that with open thoracotomy (4-6).
Uniportal VATS through intercostal space has been introduced as a less invasive alternative to the traditional multiport VATS; even so working through a single intercostal space can reduce but not completely avoid the damage of the intercostal bundle (7).
In this context the uniportal subxiphoid video-assisted thoracic surgery (SVATS) has been proposed as alternative option for a variety of thoracic procedures that could completely avoid the intercostal nerve injuries (8,9).
In Shanghai Pulmonary Hospital, after a very important experience with multiport and uniportal vats resections, we started the uniportal SVATS program for lung resection in September 2014 with very good short terms results in terms of safety, post-operative pain and morbidity (10).
The aim of this study is to describe the surgical technique used by our team for uniportal SVATS lobectomy.
Indications for SVATS lobectomy
The surgical indications were early-stage lung cancer and selected cases of localized infectious lung disease or benign lung tumor discussed within our multidisciplinary team prior to surgery.
Exclusion criteria included:
- Diffuse dense adhesion;
- Lymph nodes enlargement;
- Body mass index, BMI >30;
- Cardiomegaly patients with left-side diseases;
- Reoperation.
Operating room set up and surgical instruments
The standard set-up of the operatory room includes one monitor placed cranially above the head of the patient, the first surgeon and the scrub nurse positioned on the abdominal side of the patient with the assistant positioned on the opposite side (Figure 1).
All VATS lobectomies are performed with a 10 mm, 30 degree angled HD video-thoracoscope. The 30-degree angulation allows a good vision within the chest cavity but the use of a variable angle camera could be useful during certain part of the operation in particular the lymph node dissection.
Normal VATS instruments plus dedicated instruments specially designed for SVATS [Shanghai Medical Instruments (Group) Ltd.] are used during the operations (Figure 2).
Operative technique
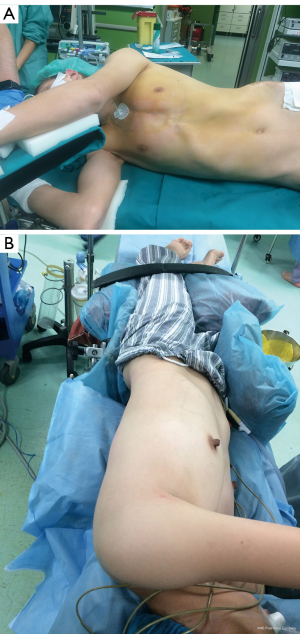
Positioning of the patients and anesthetic technique (Figure 3)
After the positioning of the double lumen tube the patients are placed in the lateral decubitus position with a backward inclination of 30° to reduce the interference deriving from the beating heart during the surgical procedure.
For left-sided operations we always put a central venous catheter line as in certain circumstances working through the subxiphoid port and pushing the pericardium can lead to circulatory instability and cardiac arrhythmias.
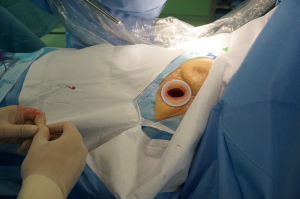
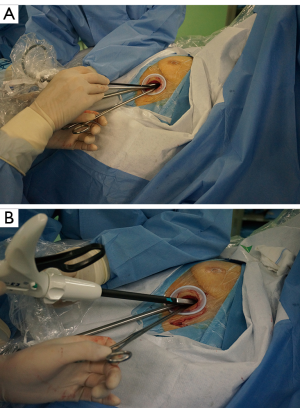
Creation of the port (Figures 4,5)

A 4-cm-long horizontal subxiphoid incision is made if the infrasternal angle is within normal limits (≥70°), otherwise a longitudinal incision is used in patients with infrasternal angle less than 70°.
At first, the subxiphoid incision is made and after dissection of the subcutaneous tissue the rectus abdominis muscle is exposed and its fibers dissected longitudinally to expose the xiphoid process that is completely resected to provide a widened operative access without lifting the sternum upward.
By index finger dissection, a retrosternal tunnel is created between the thoracic cavity, a wound protector is inserted and under thoracoscopic visualization the pleura is opened and the pericardial fat tissue is removed.
Basic surgical principles (Figure 6)
The camera is inserted through the port at the level of the caudal portion of the wound leaving the cephalic part utilizable for the insertion and the maneuver of the other surgical instruments.
In this setting is very important have confidence with the uniportal intercostal technique in order to reduce the fighting between the instruments.
The chest cavity is evaluated looking for unexpected pathology, and adhesions, and the lung is retracted using long thoracoscopic lung graspers designed to optimize the hilum exposure and reduce the interferences between the other instruments.
To reduce the interference of the heart beats is very useful the utilization of a long sucker with a distal curvature to push the pericardium medially being careful to not disturb the heart function or distort the mediastinal structure causing a reduction of the venous return.
A particularly designed long electrocautery blade is used to lift, dissect and cauterize the tissue.
The vessels, the fissures and the bronchus are exposed and divided sequentially, with appropriate endostaplers.
To transect minor pulmonary arteries, lymph adenectomy and division of thin portions of fissure we also use energy-based devices and surgical endoclips.
In case of conversion to multiport VATS an extra port is usually made at the level of the 5th intercostal space at the level of between the anterior and the middle ascellary lines while the conversion to open procedure is obtained doing a sparring muscle anterolateral thoracotomy at the 5th intercostal space level.
At the beginning of our experience we started doing a lymph node sampling but with the experience we are optimizing the technique and increasing the number of lymph nodes dissected gradually arriving to a systematic lymph node dissection with removal of lymph nodes from at least 3 N2 stations according to the IASLC/Mountain classification.
At the end of the procedure, one drain is placed in through subxiphoid incision and a thin percutaneous drain is placed at the level of the 8th intercostal space.
After surgery, the patient is transferred to an intensive postoperative care ward and, if no complications occur, the next day we proceed to the transfer to the normal ward.
We use early mobilization policy and lung physiotherapy.
The tube is removed when there is no air-leakage and less than 300 cc of fluid in 24 hours.
Patients are usually discharged one day after tube removal and seen 10 days later in the outpatient clinic.
Video atlas of uniportal subxiphoid VATS lobectomy (Figures 7-12)



Early results and comments
From November 2014 to January 2016 we performed 172 uniportal SVATS lobectomies, 126 right lobectomies and 46 left lobectomies.
We had to convert surgical approach in 12 patients (7.0%), including 5 patients (2.9%) in whom we switched to multiport VATS approach and 7 patients (4.1%) that needed thoracotomy.
The causes of conversion are indicated in Table 1.
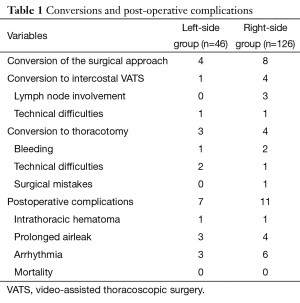
Full table
A total of 18 patients (10.5%) had postoperative complications (see Table 1), and no 30-day mortality occurred.
Even if we recognize that a more detailed analysis of the results is required to draft any statement, in our experience uniportal SVATS lobectomy for a selected category of patients showed to be a reproducible and safe alternative to the conventional multiport and uniportal lung resection techniques.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Li WW, Lee RL, Lee TW, et al. The impact of thoracic surgical access on early shoulder function: video-assisted thoracic surgery versus posterolateral thoracotomy. Eur J Cardiothorac Surg 2003;23:390-6. [Crossref] [PubMed]
- Nagahiro I, Andou A, Aoe M, et al. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: a comparison of VATS and conventional procedure. Ann Thorac Surg 2001;72:362-5. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Passlick B, Born C, Sienel W, et al. Incidence of chronic pain after minimal-invasive surgery for spontaneous pneumothorax. Eur J Cardiothorac Surg 2001;19:355-8; discussion 358-9. [Crossref] [PubMed]
- Bertrand PC, Regnard JF, Spaggiari L, et al. Immediate and long-term results after surgical treatment of primary spontaneous pneumothorax by VATS. Ann Thorac Surg 1996;61:1641-5. [Crossref] [PubMed]
- Landreneau RJ, Mack MJ, Hazelrigg SR, et al. Prevalence of chronic pain after pulmonary resection by thoracotomy or video-assisted thoracic surgery. J Thorac Cardiovasc Surg 1994;107:1079-85; discussion 1085-6. [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i37-41. [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-port thymectomy through an infrasternal approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxyphoid single-incision thoracoscopic pulmonary metastasectomy. Thorac Cancer 2015;6:230-2. [Crossref] [PubMed]
- Song N, Zhao DP, Jiang L, et al. Subxiphoid uniportal video-assisted thoracoscopic surgery (VATS) for lobectomy: a report of 105 cases. J Thorac Dis 2016;8:S251-7. [PubMed]
- Aresu G, Wu L, Jiang L, et al. Creation of the subxiphoid port. Asvide 2016;3:319. Available online: http://www.asvide.com/articles/1076
- Aresu G, Wu L, Jiang L, et al. Uniportal subxiphoid right upper lobectomy. Asvide 2016;3:320. Available online: http://www.asvide.com/articles/1077
- Aresu G, Wu L, Jiang L, et al. Uniportal subxiphoid right middle lobectomy. Asvide 2016;3:321. Available online: http://www.asvide.com/articles/1078
- Aresu G, Wu L, Jiang L, et al. Uniportal subxiphoid right lower lobectomy. Asvide 2016;3:322. Available online: http://www.asvide.com/articles/1079
- Aresu G, Wu L, Jiang L, et al. Uniportal subxiphoid left upper lobectomy. Asvide 2016;3:323. Available online: http://www.asvide.com/articles/1080
- Aresu G, Wu L, Jiang L, et al. Uniportal subxiphoid left lower lobectomy. Asvide 2016;3:324. Available online: http://www.asvide.com/articles/1081
- Aresu G, Wu L, Jiang L, et al. Uniportal subxiphoid right lower bilobectomy and lymphadenectomy. Asvide 2016;3:325. Available online: http://www.asvide.com/articles/1082
Cite this article as: Aresu G, Wu L, Lin L, Jiang G, Jiang L. The Shanghai Pulmonary Hospital subxiphoid approach for lobectomies. J Vis Surg 2016;2:135.