Diagnosis in chest wall deformities
Introduction
Congenital chest wall deformities encompass a wide spectrum of conditions. This video article discusses the protocol for accurate diagnosis of one of these conditions: pectus excavatum (PE). Most cases of PE are obvious and easily detected upon physical examination in the consultation room. PE patients present with a plethora of symptoms. A large number of these patients experience psychological distress and anxiety related to body dysmorphia. There is a unanimous feeling of body image inadequacy amongst these patients and this is often the main reason why patients present to clinicians initially. Patients may also present with varying severities of physical illness, the main one being cardiorespiratory dysfunction. The video aims to describe the necessary steps a clinician must take to reach a reliable diagnosis and how to decide on whether the patient is suitable for operative or non-operative treatment (Figure 1).
Discussion
Patients with a congenital or traumatic chest wall deformity sometimes suffer from physical illness as well as psychological distress. Symptoms of cardiorespiratory dysfunction are associated with the deformity and manifest as exercise intolerance, fatigue, decreased stamina etc. (2,3). In order to quantify the extent of the physical illness, exercise tolerance tests or lung-function tests may be carried out by the clinician. The physiological reasoning behind poor lung-function in patients suffering with PE can be explained simply by a rectangular drawing. If you split the rectangle into four triangles by drawing two lines from vertically opposite corners, intersecting at the centre of the rectangle and remove the top triangle, the area of the rectangle is reduced. This is a perfect analogy to use when explaining symptoms to a patient with PE. The rectangle can be likened to the chest cavity or the lung volume and it can be explained that the chest cavity can not rise sufficiently in order to facilitate an adequate stroke volume. Further on in this article, we will discuss indices used to quantify the extent of the chest cavity reduction.
Psychological distress is also reported as a highly prevalent symptom amongst those with PE and pectus carinatum (PC). Many patients suffer with body dysmorphia. Psychological investigation is also paramount and a full assessment of the patient’s motivations behind receiving treatment must be carried out prior to consideration for operative therapy. Further, there is a highly detailed pre-operative work-up that informs clinicians on how to make an accurate diagnosis of these two conditions.
Pectus excavatum (PE)
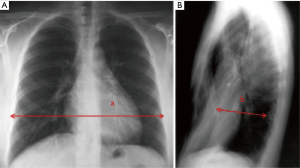
PE is the most common congenital chest wall deformity. It is characterised by posterior depression of the sternum and costal cartilages resulting in a reduction of the anteroposterior (AP) diameter of the thorax. Prior to patient selection for surgical intervention, the pre-operative work-up must be considered carefully. An important aspect of the diagnostic criteria is a measure known as the Haller index (HI). In order to interpret the HI, a CT image must be produced of the deepest part of the PE deformity. The transverse diameter and the AP diameter are quantified. The AP diameter is specifically measured from the posterior sternal surface to the anterior aspect of the vertebral body at the level of maximal depression. The ratio between these two variables is the calculated value of the HI. The diagnostic criteria suggest that operated patients on average have a HI of >3.25 and non-pectus controls have a HI of <3.25 HI (3,4). Figure 2 shows an image of chest X-ray HI measurement through two-view chest radiography. Measurements A and B correspond to the transverse diameter and the AP diameter, respectively.
Magnetic resonance imaging (MRI) may also be used to calculate HI. There is strong compatibility between using fast MRI and CT scanning with regards to the HI calculated. MRI also provides soft-tissue contrast in order for clinicians to determine cardiac displacement, rotation, great vessel anomalies and asymmetric volume between the left and right hemithorax (3).
The sternal depression index (SDI) is also sometimes calculated in order to supplement conclusions made from interpretation of HI. The SDI is measured by recording two measurements and taking the ratio between them. The first is the maximal internal sagittal diameter of the left side of the chest A. The second is the minimal distance between the anterior surface of the vertebral column and the posterior border of the deepest portion of the sternum B. The vertical distance between the higher and lowest point of the anterior chest wall is the measure of the sternal depression. Measurements A divided by B gives the SDI. An SDI of <2.4 is associated with mild sternal deformity, moderate sternal deformity is associated with an SDI of 2.4–2.9 and an SDI of >2.9 is conclusive of severe sternal deformity (5,6).
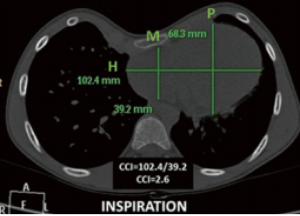
PE causes displacement of the heart into the left hemithorax. In order to measure the extent of cardiac compression, the cardiac compression index (CCI) and the cardiac asymmetry index (CAI) were derived. Figure 3 shows how to calculate CCI and CAI (5). On inspiration, H, P and M are measured from axial images of the heart. CCI is derived from H/M and CAI from P/M.
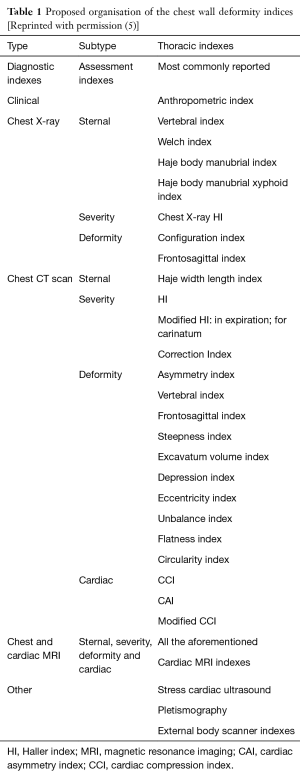
The above mentioned indices form part of a long list of measurements used to quantify the severity of sternal depression or cardiac compression through either MRI, CT or X-ray imagery. Martinez-Ferro, 2016 has proposed a classification table (Table 1) of the most commonly reported thoracic indices used clinically. To read upon most of the indices listed in the table, please consult our book Chest Wall Deformities and Corrective Procedures (5).
Full table
Echocardiography can also be undertaken to look for any valvular pathology or chamber compression. The right atrium and ventricle may be compressed by the sternum and mitral valve prolapse has been reported in up to 17% of patients with PE (3,7).
Conclusions
Clinicians are now looking for alternative ways of diagnosing PE without the use of CT Imagery. CT Imagery uses highly ionising radiation on primarily young and adolescent patients. There is therefore growing need for new measurements and indices to be discovered that can be calculated through MRI or CMR. CMR (Cardiac MRI) also provides accurate information on a patient’s cardiovascular function. This eliminates the need for echocardiography. Our centre is researching new ways of quantifying sternal depression and hope to further research in this field.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kolvekar SK, Simon N, Kolvekar T. Mr. Shyam Kolvekar’s view regarding the diagnosis of pectus excavatum (PE)—with special consideration on psychological impact. Asvide 2016;3:242. Available online: http://www.asvide.com/articles/1001
- Fonkalsrud EW. Current management of pectus excavatum. World J Surg 2003;27:502-8. [Crossref] [PubMed]
- Shukla R, Kolvekar T, Kolvekar SK. Investigations for Chest Wall Deformities. In: Kolvekar S, Pilegaard H, editors. Chest Wall Deformities and Corrective Procedures. Switzerland: Springer International Publishing, 2016:25-34.
- Baez JC, Lee EY, Restrepo R, et al. Chest wall lesions in children. AJR Am J Roentgenol 2013;200:W402-19. [Crossref] [PubMed]
- Martinez-Ferro M. Indexes for Pectus Deformities. In: Kolvekar S, Pilegaard H, editors. Chest Wall Deformities and Corrective Procedures. Switzerland: Springer International Publishing, 2016:35-60.
- Rebeis EB, Campos JR, Moreira LF, et al. Variation of the Anthropometric Index for pectus excavatum relative to age, race, and sex. Clinics (Sao Paulo) 2013;68:1215-9. [Crossref] [PubMed]
- Colombani PM. Preoperative assessment of chest wall deformities. Semin Thorac Cardiovasc Surg 2009;21:58-63. [Crossref] [PubMed]
Cite this article as: Kolvekar SK, Simon N, Kolvekar T. Diagnosis in chest wall deformities. J Vis Surg 2016;2:103.


