Video-assisted thoracoscopy the total mesoesophageal excision and systematic en bloc mediastinal lymph node dissection
Introduction
Nowadays, esophageal carcinoma is one of the malignant tumors with high incidence in China. With the rapid development of thoracoscopy, video-assisted thoracoscopy surgery has become a most reliable and primary treatment to manage esophageal cancer, and the standardized operation and radical lymph node dissection is the key of the rehabilitation and prognosis of the patients (1,2). Therefore, we believe that it’s more obvious to underline the radical cure of esophageal cancer surgery which was the total mesoesophageal excision (TME) (3-5) combined with systematic mediastinal lymph nodes complete dissection (6). In this report, we describe the TME and systematic en bloc mediastinal lymph node dissection via VATS.
Clinical summary
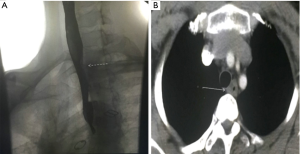
The patient was a 59-year-old woman, who was admitted into our hospital due to swallowing obstruction for over a month, and her father died of esophageal cancer. Chest computed tomography (CT) scan revealed partial thickened wall of the upper thoracic esophagus and digital gastrointestinal imaging showed the upper thoracic esophageal filling defect (Figure 1). Gastroscopy demonstrated a swelling mass that like a mushroom in 22 cm from incisor teeth, and the biopsy result demonstrated esophageal squamous cell carcinoma. The patient’s preoperative routine examinations did not reveal significant surgical contraindication.
Therefore, the TME and systematic en bloc mediastinal lymph node dissection via VATS was performed. The procedure was successful and the rehabilitation was smooth. A esophageal well differentiated squamous cell carcinoma of stage T1aN1M0 was identified on postoperative pathological examination. The postoperative examination of esophageal swallow diatrizoate meglumine and CT scan confirmed no anastomosis fistula and no signs of recurrence and metastasis.
Operative techniques
This study has obtained informed consent of patients. The patient received general anesthesia with double-lumen endotracheal intubation and left lung ventilation. She was positioned in the left recumbent position 90 degrees. The operating surgeon stood at the back side of patient, and the assistants were located in the ventral side of the patient. The first 1.5 cm incision was performed in the sixth intercostal space in the right midaxillary line, and was used for the camera. The second 3 cm long incision was made in the fourth intercostal space in the right preaxillary line for the assistant, which was used mainly to pull down lung tissue to get good exposure. The third 2 cm incision was performed in the eighth intercostal space in the scapular line and the fourth 0.5 cm incision in the seventh intercostal space in the scapular line as the operating hole. Incisions were retracted with a soft protector (Figure 2).
The first step in the procedure was to divide the inferior pulmonary ligament, and to cut open mediastinal pleura from diaphragm level, free the lower esophagus and pull up it with a tape, which revealed esophageal mesentery of the aortic side and pericardial surface. Then, the esophageal mesentery was freed with an electrical hook and ultrasonic knife from top to bottom, closely next to the pericardial surface in the front and along the thoracic aorta at the back. And we clipped the branches of esophageal arteries with titanium clips, and en bloc free the esophagus, esophageal lymph nodes and mesentery.
The second step was that we dissected the arch of azygos vein with a white Endo-GIA 30 mm vascular stapler and began to en bloc dissect mediastinal lymph nodes. The assistant fully exposed the surgical field to help the surgeon en bloc free the subcarinal lymph node. After that continued to free esophagus along the esophageal mesentery, we divided longitudinally the top of mediastinal pleura along the right vagus nerve,and exposed fully and protect the right recurrent laryngeal nerve, and completely cleaned the right recurrent laryngeal nerve paravertebral lymph nodes. Then, we lift up the upper esophagus with a 3–0 silk that set to tie the esophageal, and completely cleaned the left recurrent laryngeal nerve paravertebral lymph node. The last step in the procedure was to stop seriously the bleeding, and move the tape in the top of the chest. There was no serious morbidity that occurred in the perioperative period, and esophageal swallow diatrizoate angiography showed well healing of gastroesophageal anastomosis, and the patient was discharged after 8 days (Figure 3).

Comments
The resection of esophageal carcinoma via VATS is one of the hot topics in the study of surgical treatment of esophageal cancer, which greatly reduced the surgical trauma and improved the postoperative life quality of the patients (8). In this whole process, it’s important that the careful coordination was required between the surgical and anesthesia teams. We concluded that mesoesophagus is a special kind of organization structure that parcel in paraesophageal fatty tissue, nerves and blood vessels and lymph nodes, and which is in the same structure of dissection, and The direct metastasis and lymph node metastasis of esophageal cancer were performed along the esophagus(1,3-5). So we believe that TME and the complete resection of lymph node can improve the radical of the operation, and put forward that the surgery strategy of TME is to take mesoesophagus, vascular and lymph nodes as the core, and dissect it along the anatomical space. Therefore, it is a complete and feasible surgical procedure that TME and systematic en bloc mediastinal lymph node dissection via VATS was performed. However, this demanding procedure should be performed by experienced thoracic surgeons and in selected patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Schwarz RE, Smith DD. Clinical impact of lymphadenectomy extent in resectable esophageal cancer. J Gastrointest Surg 2007;11:1384-93; discussion 1393-4. [Crossref] [PubMed]
- Altorki NK, Zhou XK, Stiles B, et al. Total number of resected lymph nodes predicts survival in esophageal cancer. Ann Surg 2008;248:221-6. [Crossref] [PubMed]
- Tachimori Y. Total mesoesophageal esophagectomy. Chin Med J (Engl) 2014;127:574-9. [PubMed]
- Cuesta MA, Weijs TJ, Bleys RL, et al. A new concept of the anatomy of the thoracic oesophagus: the meso-oesophagus. Observational study during thoracoscopic esophagectomy. Surg Endosc 2015;29:2576-82. [Crossref] [PubMed]
- Matsubara T, Ueda M, Nagao N, et al. Cervicothoracic approach for total mesoesophageal dissection in cancer of the thoracic esophagus. J Am Coll Surg 1998;187:238-45. [Crossref] [PubMed]
- Lerut T, Nafteux P, Moons J, et al. Quality in the surgical treatment of cancer of the esophagus and gastroesophageal junction. Eur J Surg Oncol 2005;31:587-94. [Crossref] [PubMed]
- Kang M, Huang S, Lin J, et al. Video-assisted thoracoscopy the total mesoesophageal excision (TME) and systematic en bloc mediastinal lymph node dissection. Asvide 2016;3:229. Available online: http://www.asvide.com/articles/988
- Wang H, Feng M, Tan L, Wang Q. Comparison of the short-term quality of life in patients with esophageal cancer after subtotal esophagectomy via video-assisted thoracoscopic or open surgery. Dis Esophagus 2010;23:408-14. [PubMed]
Cite this article as: Kang M, Huang S, Lin J, Chen S, Lin J, Han W. Video-assisted thoracoscopy the total mesoesophageal excision and systematic en bloc mediastinal lymph node dissection. J Vis Surg 2016;2:102.



