Subxiphoid uniportal video-assisted thoracoscopic trisegmentectomy
Subxiphoid uniportal video-assisted thoracic surgery (VATS) for major lung resections is a new approach. Clinical evidence of safety and feasibility is lacking. We describe the case of a 46-year-old female who presents with recurrent cough. Computed tomography (CT) of the thorax showed two ground opacity lesions (GGOs) in the apical segment of the left upper lobe. After a subxiphoid uniportal VATS trisegmentectomy a complete resection was performed (R0 complete cancer resection on histology). Histopathologic examination showed an invasive adenocarcinoma and a minimally invasive adenocarcinoma.
Case presentation
A 46-year-old female in good general condition presented with recurrent cough of several weeks duration. No other symptoms were reported. In addition, the patient was a non-smoker and had no pre-existing conditions. Physical examination revealed no pathologic findings. Routine blood biochemistry and flexible bronchoscopy showed no abnormalities. Pulmonary lung function showed normal values of FEV1 and FVC. CT guided biopsy was negative.
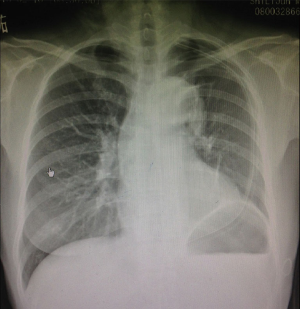
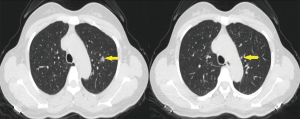
CT of the thorax showed two GGOs in the apical segment of the left upper lobe with a diameter of approximately 1.45 cm and 0.57 cm respectively (Figure 1).
All data was collected from patient notes and computer records and consent forms were signed. This new procedure and study was approved by the Hospital Institutional Review Board.
The case was performed under general anaesthesia, using single lung ventilation by one surgeon and an assistant with previous experience in uniportal VATS lobectomy. After surgery the patient was weaned from the ventilator while they were in the operating room.
The patient was put under general anaesthesia with double lumen endotracheal intubation. The patient was positioned in a lateral position at 60 to 70 degrees. A surgeon and scrub nurse stand in front of the patient. The assistant stands at the back of the patient and the screen is placed at the head of the patient. A 4 cm midline transverse incision was made below the sterno-costal triangle. The rectus abdominis was divided and xiphoid process was exposed, detached and resected from the rectus abdominis. The left pleura was opened by finger dissection and completed with electrocautery. A wound protection (Chinese Manufacture wound protector, Changzhou city, China) was placed. A 10 mm, 30-degree video camera was introduced in the lower side of the incision and the mediastinal fatty tissue around the wound was removed to facilitate the insertion of the VATS instruments in the upper side of the incision. A complete fissure was founded. The first step was the dissection of the trisegmental vein preserving the lingular vein and resected with endoscopic vascular stapler. The upper arteries including one apical branch one anterior branch and one posterior branch were dissected and resected with endoscopic vascular stapler one by one. The upper bronchus was dissected and the trisegmental bronchus was resected with endoscopic green stapler preserving the lingular bronchus. The fissure was dissected at the last stage of the lobectomy with fissureless technique to prevent air leak. After the anatomic resection, a systematic lymph node dissection was performed (Figure 2). The chest tube 28 Fr was placed at the caudal side of the incision and closed in layers starting with the muscle in the midline followed by skin. Figure 3 shows radiography of the chest 24 hours after the surgery. The mean operation time was 120 minutes and the mean operative blood loss was 80 mL, drain was removed at 3 postoperative days and patient was discharged home at postoperative day 4.
Histopathologic findings showed a 1.45×1.1×0.97 cm invasive adenocarcinoma for the large lesion (T1aN0M0) and a 0.57×0.43×0.38 cm minimally invasive adenocarcinoma for the small lesion. A complete mediastinal lymph node dissection including stations 4L, 5, 6, 7, 10 and 11 was performed with no lymph node involvement.
Comments
Subxiphoid approach has been adopted during the last 20 years for thoracic and cardiovascular minor procedures such as thymectomies, pulmonary metastasectomies, pneumothorax or pericardial windows (2-4).
In 2011 the first case of uniportal VATS lobectomy was published (5) and the aim to reduce postoperative pain and avoid intercostal nerve damage has led to the creation of the uniportal subxiphoid VATS for major lung resections, as a new technique described for the first time in 2014 (6,7). Clinical evidence of this procedure is lacking. In this case report a left upper trisegmentectomy was performed showing similar values to transthoracic uniportal VATS with regards to operating time perioperative bleeding, chest drain duration and hospital stay (8,9).
Comparing this approach with the transthoracic uniportal approach may show some disadvantages and advantages. Some disadvantages we found is that in some cases the dissection of the station 7 is very challenging and is only possible to perform sampling. When an emergent conversion to open surgery is necessary an extension of the subxiphoid incision is unlikely to be useful and an additional thoracotomy must be performed. Sometimes the instrumentation over the beating heart is problematic. Some of the advantages we found are that the subxiphoid uniportal approach may reduce the risk of intercostal nerve injury and paraesthesia because the incision is placed inferiorly to the costal margin and also potentially to avoid the limitations imposed by narrow rib spaces. One incision in the midline allows right and left access to the chest cavities in case of bilateral lesions.
Further studies are necessary to certificate the applicability and compare clinical outcomes of the subxiphoid versus the transthoracic approach, in order to show clear benefits from this technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Hernandez-Arenas LA, Lin L, Wu L, et al. The video shows how to perform a left upper trisegmentectomy and left lymph node dissection by subxiphoid uniportal approach (SVATS). Asvide 2016;3:204. Available online: http://www.asvide.com/articles/960
- Liu CY, Lin CS, Liu CC. Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 2015;10:125-8. [Crossref] [PubMed]
- Liberman M, Labos C, Sampalis JS, et al. Ten-year surgical experience with nontraumatic pericardial effusions: a comparison between the subxyphoid and transthoracic approaches to pericardial window. Arch Surg 2005;140:191-5. [Crossref] [PubMed]
- Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. [Crossref] [PubMed]
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. [Crossref] [PubMed]
- Ismail NA, Elsaegh M, Dunning J. Novel Techniques in Video-assisted Thoracic Surgery (VATS) Lobectomy. Surg Technol Int 2015;26:206-9. [PubMed]
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
Cite this article as: Hernandez-Arenas LA, Lin L, Wu L, Aresu G, Jiang G, Jiang L. Subxiphoid uniportal video-assisted thoracoscopic trisegmentectomy. J Vis Surg 2016;2:90.