Management of bleeding from an abnormally located S6 arterial branch in a common origin with S2 branch during live surgery
Text
Uniportal video-assisted thoracic surgery (VATS) is a relatively new surgical technique that was introduced at the beginning of the new millennium (1-3).
This technique was further developed and extended to major lung resections by Dr. Gonzalez-Rivas and his group in a Coruña, Spain and performed the first uniportal lobectomy in 2011 (4). Since that landmark report, he has expanded his technique to complex lung resection such as, Anatomical segmentectomies and sleeve lobectomies (5,6).
Uniportal VATS surgery has since gained popularity around the world with more and more Thoracic Surgery centers adopting this technique over the standard multi-port VATS approach.
The reason for adopting this technique throughout the world has not been because of its more appealing cosmetic result, but rather most probably because of its minimal invasiveness, surgical safety, reduced post-operative pain and shorter length of stay. These quality measures are indicators of greater efficacy compared with the standard approach.
Teaching VATS to Surgeons is a most challenging task as we are lacking effective simulators for this type of surgery. In standard VATS, the presence of the camera in a separate hole facilities the work and teaching through the working port. In uniportal VATS, the presence of camera and instruments in the same port make surgery more challenging not to mention teaching this technique.
Our group has adopted uniportal VATS as our surgical approach of choice since 2013, having transferred from standard thoracotomy directly to uniportal VATS. We use this technique exclusively in our thoracoscopic procedure. The transition learning curve through persistence, perseverance and especially the guidance of experts such as Dr. Gonzalez have allowed us to master the technique and apply it to a wide variety of procedures.
The story of adopting this technique in our institution was started after visiting Dr. Gonzalez in a Coruña (August 2013) (Figure 1) then we started immediately to perform minor cases like pneumothorax and wedge resections, then in (November 2013), Dr. Gonzalez was invited to our institution and he performed five successful cases of lobectomy during 2 days (Figure 2).

To refine our experience with this new technique we had to attend multiple important courses and meetings that were focusing on uniportal VATS in Spain, China, and Germany and this helped us to feel more comfortable to apply this technique.
In 24/03/2016 we organized the first uniportal VATS live surgery workshop in Jerusalem at our institution, more than 30 participants attended this workshop from Israeli and the Palestinian territory (cardiothoracic and vascular surgeons, general surgeons, anesthesiologists and nurses) (Figures 3,4).

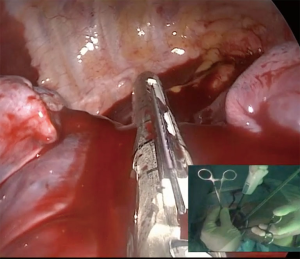
During the workshop Dr. Gonzalez operated two complex cases while the first case was an anatomical S1 segmentectomy, the second case (the one we reports in this paper) (Figure 5).
Case
We report a case of a 60 years old female with an endobronchial lesion that was found on a CT scan done due to dyspnea and cough. The CT revealed a tumor at the orifice of the right middle lobe bronchus that caused total collapse of the right middle lobe and invasion to the bronchus intermedius, transbronchial biopsy revealed a diagnosis of a typical carcinoid tumor. Ga 68-DOTATATE scan revealed an avid “2.7 cm” nodule (43 SUV) in addition to a sub carinal avid lymph node (3.7 SUV). The patient had normal lung function test (FEV1 =90%). The patient was non-smoker, had no oncological anamnesis and has some comorbidity: arterial hypertension, no-insulin dependent diabetes mellitus, hyperlipidemia and obesity (BMI >35) a decision to perform bilobectomy was taken (Figure 6).
Surgical technique
After insertion of venous cannula and arterial line, Intubation with double lumen tube was done and the patient was positioned in the lateral decubitus position. A single 4 cm skin incision was made the 5th intercostal space. The surgeon and assistant were positioned in the front of the patient. The 30° high definition thoracoscope, specially designed curved thoracoscopic instruments, and vascular polymer clips were used. During the surgery the camera was placed in the posterior part of the incision and the instruments were placed below the camera. Upon entering the cavity it became apparent that: (I) the diaphragm was very high; (II) dense adhesions of the lung to the chest wall and mediastinum; (III) small thoracic cavity.
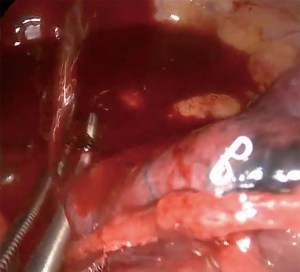
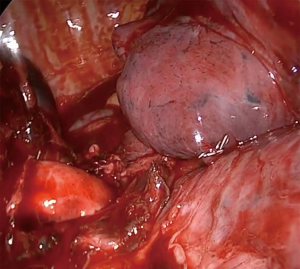
All these findings presented extreme technical difficulties with visualization, instrumentation and dissection. Isolation and separation of vascular structure and bronchus was a most daunting and difficult task, while developing the minor fissure by advancing the stapler above the main arterial trunk a profuse bleeding appeared from an abnormally located S6 (branch to the superior segment of the right lower lobe) which had arisen in a common trunk with S2 arterial branch (posterior ascending artery) (Figures 7,8), bleeding control was achieved avoiding a thoracotomy (Figures 9,10).
Lower and middle lobectomy with mediastinal lymphadenectomy was performed. The lung was extracted in a protective bag. A single chest tube was inserted through the same incision and placed posteriorly at the end of the procedure. The patient was extubated at the conclusion of surgery and transferred to the recovery ward.
The recovery of the patient was uneventful, she consumed small amounts of analgesics during her stay, mobilization started at the same day of the surgery, removal of the chest tube was done in POD #4 and she was discharged the following day.
Discussion
Coordination of all the surgical team is essential when confronting an emergency such as a major bleeding. In the event of a bleeding, it is crucial to keep calm, don’t panic and use compression and suction and the first step. Direct compression is the first measure to be taken when a bleeding occurs. The immediate manual control by means of our hands during open surgery is substituted by compression instruments in a thoracoscopic approach. At the same time it is to suck up the blood around (with long curved suction) in order to have a good the bleeding point as well as leaving a prepared field in case of the need for a later repair (8).
The suction can imitate the function of a finger compressing to stop the bleeding and allows to keep the bleeding point clear from blood. This enables a better assessment of the defect to be repaired. In addition, the curve of the suction doesn’t interfere with the suturing maneuver and the thoracoscopic view through a single-port.
The use of polymer (Click a-V, Grena®) clips can be very useful for the control of small vessel bleeding (8). When we try to place a clip over a bleeding zone we must be sure that there is sufficient surface to secure the clip at the base of the vessel. We should be extremely cautious when a clip is being applied to control bleeding because misplacement could cause irreversible damage to the pulmonary artery.
Conclusions
Control of major bleeding with uniportal VATS is feasible, effective and safe in experts’ hands. Once the experience is gained with the uniportal VATS approach the majority of the intraoperative bleedings can be controlled thoracoscopically without the need for conversion to thoracotomy. However, the conversion to open surgery should never be considered as a failure of VATS but rather as a form of guaranteeing the safety of the patient and avoid an unexpected resection.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Nesher N, Galili R, Sharony R, et al. Videothorascopic sympathectomy (VATS) for palmar hyperhidriosis:summary of a clinical trial and surgical results. Harefuah 2000;138:913-6, 1008. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5 Suppl 3:S226-33. [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-i16. [PubMed]
- Abu Akar F, Gonzalez-Rivas D, Fink D. A video of uniportal VATS lower bilobectomy with management of bleeding from an abnormally located S6 arterial branch in a common origin with S2 branch. Asvide 2016;3:203. Available online: http://www.asvide.com/articles/959
- Gonzalez-Rivas D, Stupnik T, Fernandez R, et al. Intraoperative bleeding control by uniportal video-assisted thoracoscopic surgery†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i17-i24. [PubMed]
Cite this article as: Abu Akar F, Gonzalez-Rivas D, Fink D. Management of bleeding from an abnormally located S6 arterial branch in a common origin with S2 branch during live surgery. J Vis Surg 2016;2:87.