Left upper lobectomy with bronchoplasty in uniportal video-assisted thoracic surgery for bronchial carcinoid
Introduction
Uniportal video-assisted thoracic surgery (VATS) has become an increasingly popular approach to manage thoracic surgical diseases, because of the reduced access trauma and better cosmesis. A major milestone for this approach came in June 2010 in the form of the world’s first uniportal VATS lobectomy, which was subsequently reported in 2011 by Gonzalez Rivas (1). Since then, complex uniportal VATS lung resection involving pneumonectomy, segmentectomy and chest wall resection have been successfully accomplished (2,3).
However, reports of lobectomy with bronchoplasty in uniportal VATS are extremely rare (4,5). In this report, I describe a left upper lobectomy with bronchoplasty in uniportal VATS for bronchial carcinoid.
Clinical summary
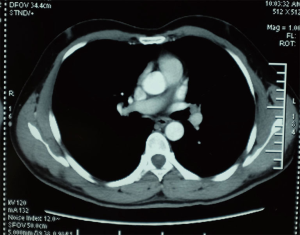
A 36-year-old male smoker presented with a bronchial carcinoid. Chest computed tomography (CT) shows a carcinoid tumour in the left upper lobe (LUL) associated with bronchial occlusion of the LUL bronchus (Figure 1). Bronchoscope examination shows a neoplasm in the orifice of LUL bronchus (Figure 2). The biopsy result demonstrates bronchial carcinoid.
A left upper lobectomy with bronchoplasty was performed through a 3.5 cm single-incision in vats (Figure 3). The total operating time was 292 min. The procedure was successful and the recovery uneventful. The patient’s chest tube was removed on the 5th day, and he was discharged home on the ninth day. Pathological examination revealed a carcinoid tumor with no lymph node involvement (T1bN0M0). The follow-up bronchoscopy and CT scan confirmed no stenosis and no signs of recurrence.
Operative techniques
This study has obtained informed consent from the patient. The patient was placed in the lateral decubitus position. The surgeon stood at the patient’s right side, and a 3.5 cm incision was made at the fifth intercostal space on the anterior axillary line with no rib spreading. We used a 10-mm high-definition 30-degree thoracoscope to adequately visualize the working field through the small single incision. The camera was placed in the posterior portion of the incision with instruments inserted parallel to and below the camera. All procedures were performed while viewing the monitors. The lobectomy is done through an anterior approach where the surgeon stands in front of the patient with the assistant and scrub nurse on the opposite side.
Pulmonary vessels were resected as for standard lobectomy. Mediastinal lymph nodes, including the subcarinal nodes, were also dissected before bronchial reconstruction.
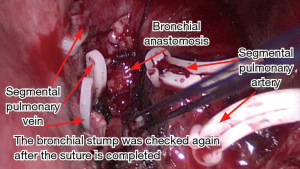
A left upper lobectomy was performed leaving the bronchus as the last step of the procedure. The left lower lobe bronchus was dissected and exposed. The LUL bronchus was cut wedge wise with a knife and scissors and the lobe was removed in a protective bag, and then the bronchial stump was confirmed by frozen sectioning to be pathologically free of cancer. After careful retraction of the artery stump, we performed the bronchial anastomosis in wedge plasty with several interrupted 3–0 absorbable mono-filament sutures (Figure 4). Both sutures were tied with the help of a thoracoscopic knot-pusher. The anastomosis was not buttressed. The remaining lung was re-expanded and the anastomosis was checked for an air leak under water and if fistulae of the bronchioles were found, they should be sutured. Bronchoscopy was performed to confirm that there was no stenosis after completion of the anastomosis. A single chest tube was placed through the incision (Figure 3).
Comments
Uniportal VATS follows the same principles of coordination as in open surgery, since the camera is usually placed at the posterior part of the incision and the instruments performing the procedure are always bellow, mimicking the eye-hand position and coordination of open surgery (6).
Video-assisted thoracoscopic surgery lobectomy with bronchoplasty is a safe and feasible surgical approach in the treatment of non-small cell lung cancer. The operating incision placed at the 5th intercostal space on the anterior axillary line is convenient for anastomosis. A full-thickness interrupted suture was used in bronchial anastomoses.
Lobectomies with bronchoplasty are among the most complex cases in thoracic surgery, even in open surgery these cases are usually challenging for thoracic surgeons. The success in performing uniportal complex VATS lobectomies is a result of skills and experience accumulated over time from performing uniportal VATS surgery. We believe that by avoiding the use of the trocar, the possibility of an inter-costal nerve injury could be minimized in comparison with conventional VATS.
Acknowledgements
The study was supported by the fund of six peak talents in Jiangsu Province (No. 2012-WS-115).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
- Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Wang BY, Tu CC, Liu CY, et al. Single-incision thoracoscopic lobectomy and segmentectomy with radical lymph node dissection. Ann Thorac Surg 2013;96:977-82. [Crossref] [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Left lower sleeve lobectomy by uniportal video-assisted thoracoscopic approach. Interact Cardiovasc Thorac Surg 2014;18:237-9. [Crossref] [PubMed]
- Guido W, Gonzalez-Rivas D, Duang L, et al. Uniportal video-assisted thoracoscopic right upper sleeve lobectomy. J Vis Surg 2015;1:10.
- Gonzalez D, de la Torre M, Paradela M, et al. Video-assisted thoracic surgery lobectomy: 3-year initial experience with 200 cases. Eur J Cardiothorac Surg 2011;40:e21-8. [Crossref] [PubMed]
Cite this article as: Zhang Z, Yuan F, Yin R, Xu L. Left upper lobectomy with bronchoplasty in uniportal video-assisted thoracic surgery for bronchial carcinoid. J Vis Surg 2016;2:84.